Intravenous (IV) line management is critical for patient safety, yet disorganized practices often lead to medication errors, infections, and extended hospital stays. Studies show that 56% of medication errors involve IV drugs, with errors five times more likely compared to other administration methods. Poor IV handling can increase hospital costs by up to $4,000 per patient and raise mortality risks. Standardizing line management protocols can significantly reduce these risks while improving workflow efficiency.
Key takeaways:
- Medication errors: IV drugs account for 56% of errors, 73% of which involve incorrect administration rates.
- Complications: Up to 42% of catheter insertions result in issues like phlebitis or infections.
- Cost impact: IV complications increase hospital stays and costs by 57%.
- Solutions: Effective systems include clear protocols, staff training, and monitoring tools like real-time alerts and line organizers.
A practical example is the Beata Clasp, a tool designed to organize IV tubing, which reduced medication errors by 35% in one hospital. Implementing facility-wide systems requires leadership support, addressing staff resistance, and tailoring approaches for different units. Continuous monitoring and data-driven adjustments are essential for sustained success. Ultimately, improving IV line management enhances patient safety and reduces healthcare costs.
How To Maintain An IV Line? - Nursing Knowledge Exchange
Core Components of an Effective Line Management System
A strong IV line management system is built on essential components that prioritize patient safety and address challenges like the high IV failure rate of 53%.
Standard Protocols for IV Line Handling
Clear, standardized protocols are critical to preventing complications caused by inconsistent practices.
Hand hygiene is the foundation of safe IV line management. Staff must clean their hands before and after touching catheter insertion sites, as well as before and after inserting, replacing, accessing, repairing, or dressing an IV catheter.
Aseptic techniques are non-negotiable. Skin preparation before inserting a peripheral catheter should involve 70% alcohol, tincture of iodine, or alcoholic chlorhexidine gluconate. For central venous or peripheral arterial catheters, use a chlorhexidine solution with more than 0.5% alcohol both during insertion and when changing dressings.
Regular site monitoring and maintenance help catch issues early. Daily checks should include palpating for tenderness and inspecting transparent dressings. Replace any dressing that becomes damp, loose, or dirty, and avoid exposing the site to water.
Catheter securement is equally important. Sutureless securement devices minimize infection risks, and protocols should stress removing catheters as soon as they’re no longer needed.
These protocols are only effective when paired with consistent and thorough staff training.
Staff Training and Skills Assessment
Even the best protocols rely on skilled, well-trained staff who are regularly evaluated.
Scenario-based learning offers practical training opportunities. Emergency drills that simulate IV-related complications help staff prepare for real-life situations.
Annual competency assessments ensure staff skills stay sharp. These evaluations should test both theoretical knowledge and hands-on abilities, with refresher sessions provided as needed.
Specialized training programs can lead to better outcomes. For instance, vascular access teams (VATs) trained in advanced techniques, like ultrasound-guided insertion, can reduce the need for central venous catheter placement by up to 80%.
Technology-focused training is also key. Staff should be proficient in using tools like ultrasound devices and smart infusion pumps to improve IV placement accuracy and identify potential issues early.
Once protocols and training are in place, monitoring systems ensure compliance and identify risks.
Monitoring Tools and Systems
Effective monitoring tools are essential for maintaining protocol compliance and addressing risks before they become serious.
Real-time monitoring technology helps manage IV therapy more effectively. Systems at nursing stations can alert staff to problems like occlusions or empty IV bags.
Automated checklists streamline pre-infusion evaluations. These tools help identify high-risk situations during the patient assessment phase.
Incident reporting systems provide valuable data. Real-time software tracks complications and supports evidence-based improvements in IV line management.
Performance improvement bundles combine several monitoring tools and interventions to promote adherence to best practices.
Patient engagement tools empower patients to play a role in their own care. Educational materials and pre-treatment briefings help patients recognize warning signs and report any discomfort or changes at the catheter site.
Remote monitoring applications enhance precision. These tools can track IV infusion rates, ensuring accurate dosage delivery and reducing medication errors. In hospital settings, they also help staff manage individualized IV schedules by sending timely reminders.
How to Implement a Facility-Wide Line Management System
Rolling out a facility-wide IV line management system takes careful planning, strong organizational commitment, and a step-by-step approach to solving challenges.
Getting Staff and Leadership on Board
Gaining the support of both frontline staff and senior leadership is crucial to making patient safety a top priority.
"Successful implementation and sustainment of the CANDOR process requires the entire organization's input, support, and buy-in."
Start by creating a compelling business case that ties the program to your organization's goals for patient safety and quality improvement. Use concrete data - like current IV-related complications and their costs - to highlight the potential benefits. Framing the initiative within the organization's broader strategic goals can also help build alignment.
Early involvement of staff and leadership fosters a sense of ownership and reduces resistance to change. Host meetings or workshops to explain the changes, why they’re necessary, and how they’ll benefit both patients and staff. Use clear, relatable language to ensure the message resonates across all levels of the organization.
A great example comes from a Chief Nursing Officer (CNO) who involved nurses in tackling pressure ulcers. By promoting shared ownership and maintaining open communication, the team achieved an 85% reduction in cases.
Regular meetings between senior leaders and teams also help strengthen collaboration and provide a forum to address setbacks.
Once leadership and staff are on the same page, the next step is tackling the challenges that come with implementation.
Solving Common Implementation Problems
After securing commitment, focus on addressing common hurdles systematically.
Resistance to change often stems from unfamiliarity. To counter this, offer ongoing education, positive reinforcement, and hands-on training to build confidence and skills. Empower enthusiastic team members by assigning them leadership roles in specific areas of the rollout.
Confusion about new protocols can lead to compliance issues. Promoting a Just Culture - where staff can report errors without fear of punishment - encourages open discussions about challenges and near-misses.
Resource limitations can derail even the best plans. Create a focused strategy to address known barriers in IV line management, maximize internal resources, and consider starting with a small pilot program to demonstrate success.
Breakdowns in communication between departments can fragment efforts. To avoid this, set up regular interdisciplinary meetings and use multiple communication channels - like emails, flyers, or dedicated sections on internal websites - to share updates clearly and consistently.
Deploying the System Across Different Units
Each care setting has unique needs, so tailor your approach for different units while sticking to core principles.
- ICUs: Focus on advanced training and monitoring protocols. ICU teams are more likely to adopt changes when the safety benefits are evident.
- Medical-surgical units: Use adaptable protocols that account for different acuity levels while maintaining standardized best practices. Visual aids and decision trees can simplify interventions.
- Emergency departments: Streamline protocols to fit seamlessly into triage and treatment workflows. Tools like mobile sterile compartment trays and point-of-care training materials can support quick, effective decision-making.
- Pediatric units: Develop age-appropriate protocols, involve child life specialists, and provide family education to ensure the best outcomes.
- Home care environments: Adapt protocols for settings with limited immediate support. Provide clear patient and caregiver education materials, establish reliable communication channels, and create simple troubleshooting guides.
One example of success comes from a pediatric emergency room initiative that used low-cost mobile sterile compartment trays, audit systems, and infection control nurses to reduce infiltration rates from 82.9% to 45% and phlebitis from 96.1% to 55%.
"Multifaceted QI IV line insertion and maintenance bundle reduced the incidence of infiltration and phlebitis. These interventions when integrated into daily work bundles along with continuous education and motivation help in sustaining the goal and attaining long-term success."
– Neelima Singh, Department of Nursing, Vardhman Mahavir Medical College and Safdarjung Hospital
Celebrate staff contributions with formal recognition and regular progress reviews to keep the momentum going.
A successful facility-wide implementation requires persistence and flexibility. Stay connected with senior leaders about upcoming priorities and be ready to revisit challenges as needs evolve.
sbb-itb-f779e18
Tools and Products for Better Line Organization
Effective IV line management is essential in healthcare settings, and the right tools can significantly improve safety and efficiency at the bedside. IV line organizers simplify the process by creating a clear system for managing multiple lines, reducing risks, and turning cluttered setups into well-organized, safer spaces.
How IV Line Organizers Reduce Risks
IV line organizers tackle some of the most pressing safety challenges in acute care. When multiple lines are present, tangled tubing can pose risks for both patients and staff. As one expert explained:
"Organizing IV lines is important for clinical staff to quickly identify solutions and keep lines at eye level and off the floor to minimize trip hazards or accidental dislodgment." – OTEN Medical
By providing a clear visual separation between lines, these organizers help reduce medication errors. Neatly arranged tubing allows nurses to quickly identify and trace the correct line during medication administration. A real-world example comes from Massachusetts General Hospital, where, between January and June 2024, introducing a standardized IV line organizer system in three ICUs led to a 35% drop in medication errors, a 42% reduction in line obstructions, and a 28% increase in time spent on direct patient care.
Keeping tubing off the floor also prevents contamination, maintaining the sterile integrity of IV systems. Plus, by eliminating the hassle of untangling lines, nurses can spend more time focusing on patient care. When choosing an organizer, healthcare providers should prioritize features like clear line separation, ease of use, enhanced visibility, and a durable, flexible design.
One standout product in this space is the Beata Clasp.
Beata Clasp Features and Benefits
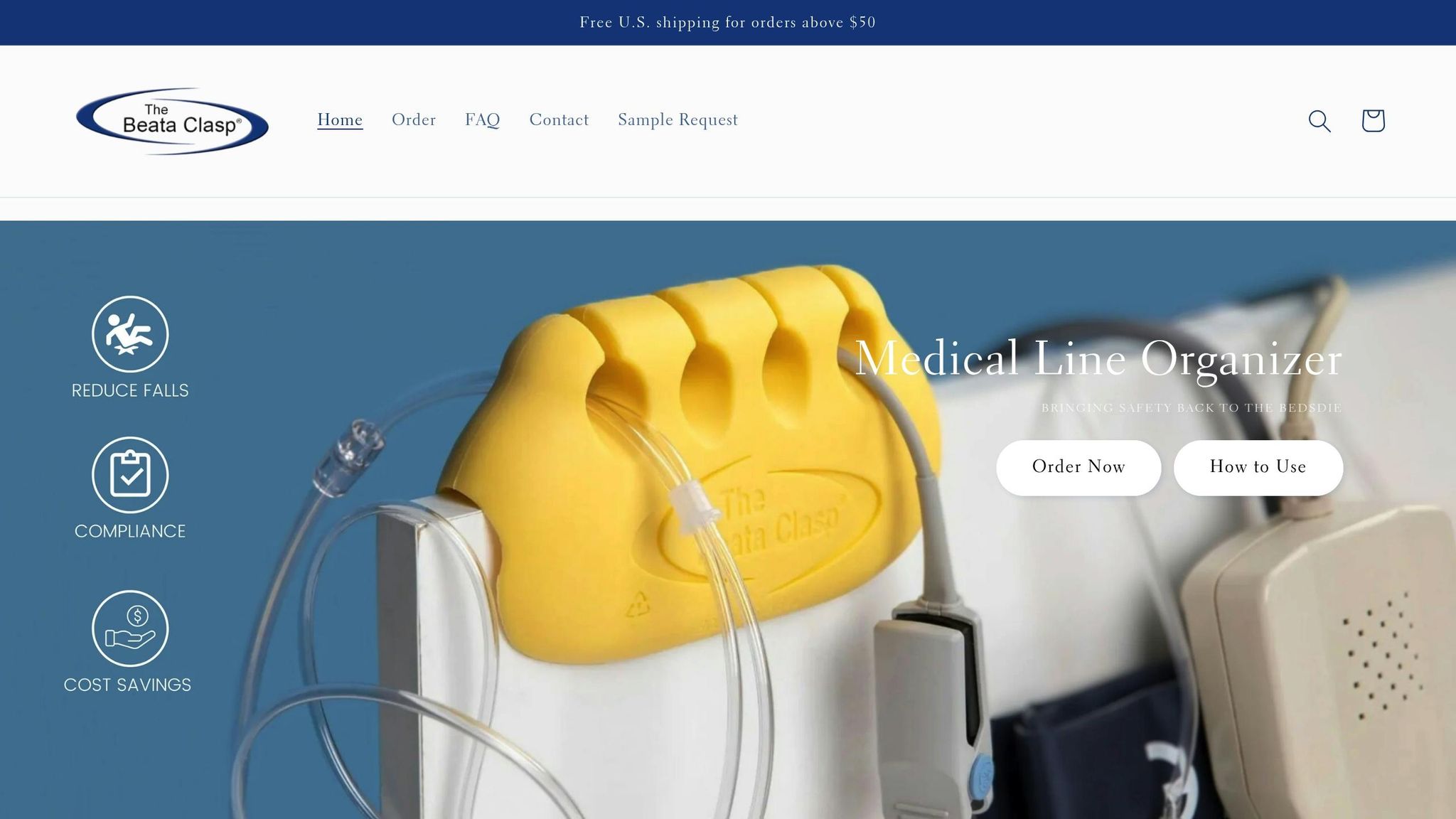
The Beata Clasp is designed to address the common challenges of tangled IV lines, improving both safety and workflow efficiency. Its circular grooves securely hold tubing and catheters in place, minimizing risks like line impingement, dislodgment, entanglement, and contamination. The product’s antimicrobial properties enhance infection control, while its bright yellow color ensures quick and easy identification. With the ability to manage multiple lines simultaneously, the Beata Clasp simplifies tracing lines back to their source.
A study conducted at Rush-Copley Medical Center highlighted its effectiveness. Nurses reported no incidents of line or tubing issues among patients using the Beata Clasp, compared to two incidents in the control group where tangled lines required intervention. Additionally, every nurse in the study expressed satisfaction with the product and a willingness to recommend it to colleagues.
The Beata Clasp is also designed with sustainability in mind. It’s latex-free, recyclable, and lightweight, making it a practical choice for various settings, from ICUs to home healthcare environments.
Beata Clasp Pricing and Purchase Options
BeataClasp offers a range of pricing options to suit different needs:
| Option | Price | Best For |
|---|---|---|
| Individual Unit | $21.95 | Small-scale testing or specific patient needs |
| Beata Clasp + Fastener | $22.95 | Added securing capabilities |
| Mini Evaluation Pack (3 units) | $60.00 | Initial product testing |
| 4 Hole Yellow Bulk Orders | From $587.50 | Large-scale facility use |
| Reusable Fastener Ties | $0.99 | Maintenance supplies |
For facilities looking to implement the Beata Clasp on a larger scale, the Line Management Awareness Program Bundle is available for $5,000.00. This comprehensive package includes training materials, staff education resources, and 100 Beata Clasp units with fasteners, helping standardize line management practices and promote safer bedside care.
Healthcare facilities can purchase the Beata Clasp through Amazon Business, local distributors, or direct purchase orders. International distributors are also available for streamlined procurement.
The Beata Clasp’s value becomes evident when considering the potential cost savings from reduced medication errors, fewer contamination incidents, and improved nursing efficiency. Bulk orders offer significant per-unit savings, while evaluation packs allow facilities to test the product’s effectiveness before committing to a larger rollout.
Tracking Success and Making Improvements
Rolling out a facility-wide IV line management system is just the beginning. The real challenge lies in maintaining and improving safety standards over time. To truly elevate bedside safety, healthcare facilities need to continuously monitor performance and refine their practices. Without consistent tracking, opportunities to improve patient outcomes and streamline operations might slip through the cracks. By combining standardized protocols with ongoing staff training, tracking key metrics ensures progress remains steady.
Key Metrics to Track
Several metrics are essential for evaluating the effectiveness of IV line management systems:
- Infection Rates: Monitor rates of infections like CLABSI and CAUTI. For instance, data from the first quarter of 2024 indicated that infection rates had dropped compared to pre-pandemic levels.
- Medication Errors: Tracking both the frequency and severity of medication errors provides a clear picture of the system’s safety impact.
- Staff Compliance: Measure adherence to protocols such as IV line insertion techniques, maintenance schedules, and drug administration checklists. Compliance data, like checklist completion rates, offers valuable insights into how well staff are following procedures.
- Complication Rates: IV failure rates can be alarmingly high - up to 53% - with infiltration incidents being a major concern.
- Patient Outcomes: Metrics like patient satisfaction scores, average hospital stays, and readmission rates help assess the broader impact of improved IV line management on both patients and facility operations.
Before and After Implementation Audits
Clinical audits are a cornerstone of measuring progress. By comparing practices before and after implementing a new IV line management system, facilities can clearly see the impact of their efforts. These audits evaluate current practices against evidence-based standards, highlighting areas of improvement.
For example, a neonatal intensive care unit saw significant changes after introducing enhanced surveillance and prevention strategies. Initially, IV complication rates were five per 1,000 line days. Post-intervention audits showed an increase to nine per 1,000 line days, reflecting better detection rather than an actual rise in complications. Most importantly, severe Stage 4 infiltrates decreased noticeably, demonstrating the effectiveness of the new protocols.
Consistency in audit methods is key. Conducting regular audits ensures sustained improvements and helps identify any backsliding. One study found complication rates fluctuating dramatically between audit rounds, ranging from 7.8% to 39%. These variations underscore the importance of ongoing and detailed evaluations to guide targeted interventions.
Using Data to Make Ongoing Improvements
Insights from audits and metric reviews should drive continuous refinements. For example, analyzing electronic medical records (EMR) can reveal inefficiencies and guide improvements.
A case study from Sheikh Shakhbout Medical City in Abu Dhabi illustrates this well. Over seven months, a retrospective analysis of 311 patients with difficult IV access (DIVA) revealed that 74.6% had a documented history of access challenges. This led to the creation of structured escalation pathways and advanced nurse training programs, boosting first-attempt success rates to 68.8%. Addressing DIVA through such strategies is crucial for improving outcomes.
Predictive analytics can further enhance these systems. By identifying high-risk patients early, staff can allocate resources more effectively and prevent complications before they arise. Regular data review sessions with stakeholders also help uncover practical solutions and ensure resources are directed where they’re needed most.
Focusing on high-demand areas - such as wards with consistently higher complication rates - can make a big difference. Ongoing monitoring plans, combined with regular analyses, help maintain progress over time and catch emerging trends before they become issues.
Conclusion: Creating a New Standard in Bedside Safety
Adopting a facility-wide IV line management system represents a major step toward delivering safer and more efficient care. Consider this: IV infusions are linked to 54% of all adverse drug events, 56% of medication errors, and 61% of serious, life-threatening errors. Beyond enhancing safety, these improvements also bring considerable financial and operational advantages.
Healthcare facilities that implement standardized systems often see cost reductions between 10% and 30%. With medication errors costing an estimated $42 billion annually, the financial incentive for comprehensive IV line management is clear. Patients facing IV-related complications typically stay in the hospital longer - about six days compared to under four for those without issues - and rack up higher costs, averaging nearly $11,000 versus $7,000 for patients without complications.
Sustainable improvements come from combining standardized protocols with practical tools and a supportive culture. The Beata Clasp is a great example of this - a nurse-designed solution that tackles bedside challenges without requiring costly tech upgrades. For instance, IV-oncology medication administration times dropped from over six minutes to just 41 seconds when these systems were in place. While tools like the Beata Clasp deliver immediate results, ongoing staff training and vigilance are key to maintaining progress.
True success lies in a commitment to continuous improvement. Leading organizations approach patient safety as a collaborative effort, blending leadership, teamwork, and regular practice adjustments rather than relying on any single solution. Frequent monitoring, comprehensive training, and data-informed updates ensure that initial gains are not only maintained but expanded over time.
FAQs
How can a facility-wide IV line management system enhance patient safety and lower healthcare costs?
Implementing a thorough IV line management system throughout a healthcare facility can greatly improve patient safety. It helps cut down medication errors, prevents adverse drug events, and reduces the risk of infections. These changes not only protect patients but also lead to better recovery rates, shorter hospital stays, and fewer complications.
Beyond safety, this system can have a major impact on costs. By reducing the need for corrective treatments and making workflows more efficient, facilities can save a substantial amount of money - potentially over $144,000 in just three months. This strategy benefits patients while also ensuring smoother operations and stronger financial stability for the facility.
What are the essential parts of an IV line management system, and how do they help prevent complications?
An effective IV line management system depends on several essential components working together seamlessly to maintain safety and efficiency. These components include sterile spikes and tubing, catheter hubs, needleless connectors, syringes, drip chambers, roller clamps, injection ports, and Y-sites. Each piece serves a specific purpose, from ensuring sterile connections to regulating fluid flow and providing easy access for delivering medications or fluids.
When healthcare providers follow proper site assessments, use sterile techniques, apply securement devices, and perform routine monitoring, they can greatly reduce risks such as infections, occlusions, phlebitis, or device-related injuries. This approach not only prioritizes patient safety but also streamlines workflows for medical teams, making care delivery smoother and more effective.
What are the best strategies for overcoming challenges when introducing a standardized IV line management system across different units?
Healthcare facilities can tackle the hurdles of implementing a standardized IV line management system by focusing on a few practical approaches:
- Provide comprehensive staff training: Equip your team with the necessary knowledge and hands-on skills to handle IV lines effectively. Consistency across units should be a priority to ensure smooth operations and minimize errors.
- Establish clear protocols: Design straightforward, step-by-step guidelines that simplify the process of organizing and maintaining IV lines. This can help reduce mistakes and streamline workflows.
- Work within resource limitations: Opt for budget-friendly tools and solutions that align with your facility's unique needs. This ensures the system remains practical and usable across all departments.
Focusing on these strategies can boost patient safety, cut down on infection risks, and improve the overall efficiency of IV line management processes.
