Managing multiple IV lines is crucial but comes with risks like medication errors, infections, and equipment issues. These errors can extend hospital stays by 2 days, costing up to $4,000 more per patient. Here's what you need to know to reduce these risks:
- Medication Errors: 22.6% of IV line errors involve mix-ups, with high-alert drugs like heparin and insulin often affected.
- Infections: Each additional IV line increases infection risks, costing hospitals $6,000 per bloodstream infection.
- Equipment Issues: Tangled lines and attachment failures occur in up to 14.6% of cases, delaying care.
Solutions:
- Organize IV Lines: Use tools like multi-port connectors and IV organizers (e.g., Beata Clasp) to reduce tangling and errors.
- Label Clearly: Color-coded, standardized labels help prevent mix-ups.
- Regular Maintenance: Hourly checks and proper hygiene lower infection risks.
Quick Tip: Studies show that using IV organizers and clear labels can eliminate infusion errors and save time in critical care settings.
How To Manage IV Therapy Complications? - Nursing Knowledge Exchange
Common IV Line Risks in Multi-Line Setups
Handling multiple IV lines introduces a range of safety challenges that can impact both patient outcomes and clinical workflows. The more lines involved, the greater the potential for complications.
Medication Errors and Line Mix-ups
Mixing up IV lines is a serious concern, occurring in 22.6% of all IV line errors. When multiple infusions are running simultaneously, the risk of pairing the wrong medication with the wrong line increases significantly.
High-alert medications are involved in the majority of these errors, accounting for 71% of infusion mistakes and 92% of line mix-ups. Among the most frequently implicated drugs are heparin (16%), insulin (7.6%), and parenteral nutrition (5.2%). Intensive care units (ICUs) are especially prone to such errors, with 30% of all IV line mistakes reported in these high-pressure environments.
Higher Risk of Infection
Using multiple IV lines creates additional entry points for pathogens, which raises the risk of infections. Frequent handling of these lines further increases the likelihood of contamination. Each bloodstream infection can cost hospitals an estimated $6,000 and extend a patient's stay by about seven days. While the overall rate of IV line infections from central lines in hospitalized patients is around 1%, the risk is significantly higher in critical care settings. Disorganized IV setups can make it harder to maintain proper aseptic techniques, further compounding the risk of contamination.
Equipment Problems
The more IV lines in use, the higher the likelihood of equipment-related issues. Problems such as attachment failures (14.6% of errors) and piggyback infusion complications (12.8% of errors) become increasingly common. These challenges highlight the importance of keeping IV setups well-organized and conducting regular safety checks to minimize risks.
Main Causes of IV Line Problems
Understanding the root causes of IV line issues is essential for reducing risks and improving patient safety. Several factors make managing multiple IV lines particularly challenging, increasing the chances of errors that can have serious consequences.
Complex Equipment Setups
The more intricate the IV system, the greater the potential for errors. Multi-line IV setups often involve a tangle of pumps, connectors, stopcocks, and tubing systems, making them difficult to manage effectively. These setups are especially problematic in high-pressure environments like ICUs, where quick decisions are critical.
This complexity isn’t just a logistical headache - it’s costly. Infusion-related errors contribute an estimated $2 billion annually to U.S. healthcare costs. Each additional piece of equipment introduces a new point where something could go wrong, potentially disrupting medication delivery and putting patients at risk.
For healthcare teams, managing these technical setups is a balancing act. Keeping track of the equipment while ensuring accurate medication administration can be overwhelming, especially in fast-paced settings.
Difficulty Following Lines
One of the biggest challenges with multiple IV lines is tracing them accurately from start to finish. Known as line entanglement, this issue arises when lines become tangled, making it hard to identify which line corresponds to which medication or infusion.
A single patient might have anywhere from five to seven IV lines - or even as many as 15 in extreme cases. Tracing these lines can take up to five minutes, a delay that healthcare professionals can’t afford during emergencies. Misidentifying a line can lead to errors, such as administering the wrong medication or adjusting the wrong infusion.
Studies in simulated ICU settings reveal just how common these mistakes are. For instance, 7.7% of errors occur while screening IV lines to confirm proper infusion identification. These errors emphasize the risks posed by visual confusion, particularly in high-stakes situations.
Lack of Standard Practices
Beyond the physical challenges, inconsistent practices in IV line management further increase the risk of errors. When healthcare staff rotate between units with varying protocols, the lack of standardization can lead to confusion and mistakes.
Labeling practices are a prime example of this inconsistency. Research shows that 95% of healthcare workers do not consistently label IV lines, and when labeling is done, it’s often incomplete or incorrect. Additionally, 29.6% of respondents reported that their workplace lacked a standard protocol for IV-line labeling. This lack of uniformity leaves room for preventable errors.
Data from Pennsylvania highlights the scope of the problem. Between 2004 and 2013, there were 907 reported medication errors related to IV-line management. Common mistakes included setting incorrect infusion rates and mishandling disordered lines. Alarmingly, 71% of these errors involved medications with potentially serious consequences.
The COVID-19 pandemic has only made these challenges more pronounced. With many patients requiring multiple drips simultaneously, the absence of standardized practices for organizing, labeling, and managing IV lines has further strained healthcare teams. Consistent protocols could help mitigate these risks, but without them, errors remain a persistent threat.
sbb-itb-f779e18
Proven Ways to Reduce IV Line Risks
Healthcare facilities in the United States have adopted specific strategies to minimize IV line complications and improve patient care. These approaches emphasize better organization, clear labeling, and consistent maintenance of IV lines, particularly in settings where multiple lines are in use.
Multi-Port Connectors
Multi-port connectors simplify the management of multiple IV lines by consolidating them into a single, streamlined system. This reduces the risk of leaks, disconnections, and line mix-ups. In intensive care units, where numerous IV lines are common, these connectors help prevent tangling and ensure medication flows smoothly. By reducing mechanical complexity, staff can more easily manage and monitor infusions. Pairing these connectors with clear labeling further enhances the system's efficiency and safety.
Clear Labels and Line Organization
Proper labeling is a small yet crucial step in ensuring IV line safety. Using color-coded labels makes it easier to identify medications instantly. These labels should be placed on each distal port and along the tubing to allow quick identification at every critical point. Standardized labeling practices across healthcare facilities significantly improve safety outcomes.
Michael Ganio, Pharm.D., M.S., BCSCP, FASHIP, and Senior Director of Pharmacy Practice and Quality at ASHP, highlights the importance of labeling:
"It's all the information you need to know what drug is in that line."
To avoid confusion, labels should vary in color, size, and font. Distinct lettering formats are especially helpful in preventing errors with drugs that look or sound alike. Ongoing staff education is key to maintaining consistent labeling practices.
The consequences of improper labeling are serious. In UK hospitals and long-term care facilities, IV administration errors have been reported at a rate of 53 percent. With nearly 80 percent of hospital patients receiving IV treatments during their stay, incomplete or unclear labeling poses a significant risk to patient safety.
Regular Line Checks and Maintenance
Once connectors are organized and labels are in place, regular checks and maintenance are essential to complete the safety process. Staff should inspect IV sites hourly for signs of complications such as temperature changes, leakage, or swelling. These checks help detect issues like infiltration, extravasation, or infections early on .
Routine maintenance, including changing IV tubing and dressings at recommended intervals, is critical to reducing infection risks. Preventing vascular catheter-associated infections, a common and preventable hospital-acquired condition, underscores the importance of these protocols.
Proper hand hygiene before handling IV equipment is another basic yet vital step in preventing contamination. If any equipment or solution becomes contaminated, it should be replaced immediately to avoid introducing bacteria into the system.
The table below outlines common complications, their signs, and immediate actions:
| Complication | Signs and Symptoms | Immediate Action |
|---|---|---|
| Phlebitis | Redness, pain, heat, swelling | Remove cannula, elevate arm, apply warm compress |
| Infiltration | Pain, swelling, cool skin, redness | Stop infusion, remove cannula |
| Extravasation | Burning, stinging, redness, necrosis | Stop infusion, remove cannula, follow policy |
| Local Infection | Purulent drainage at the site | Remove cannula, clean site with sterile technique |
Educating patients and caregivers is equally important. They should be encouraged to report any discomfort, tingling, or numbness at IV sites. Keeping IV sites dry, visible, and secure during movement helps maintain the system's integrity and prevents complications.
Tools like the BeataClasp IV line organizer also contribute to safety. By keeping lines off the floor and organized, it reduces contamination risks and simplifies routine checks. Its antimicrobial, latex-free, and easy-to-clean features align with infection control protocols. Additionally, its high-visibility design allows healthcare staff to assess lines quickly and efficiently during regular inspections.
How IV Line Organizers Improve Patient Safety
Managing multiple IV lines can be a logistical nightmare, but IV line organizers offer a practical solution. These tools not only simplify the process but also create a safer environment for patients while lightening the workload for healthcare staff. They go beyond just keeping things tidy - helping to control infections, ensure medication accuracy, and boost overall patient care. This targeted approach has inspired innovations designed to address these risks effectively.
How IV Line Organizers Reduce Risks
IV line organizers tackle several safety challenges head-on. By keeping lines untangled and medications clearly separated, they help prevent delays and dangerous mix-ups. Tangled IV lines can eat up valuable time as healthcare workers struggle to sort them out - time that could be better spent on direct patient care. In critical situations, this disorganization can lead to delayed treatments and heightened stress.
These tools also address the alarming risks of medication errors in setups with multiple IV lines. Research shows that 48% of incidents involving such errors were classified as harm score D or higher, with 6.2% reaching harm score E or greater. Even more concerning, nearly all (95%) of these errors made it to the patient.
By creating a streamlined system, IV line organizers make it easier for medical staff to quickly identify and manage infusions. This is especially important in fast-paced environments like hospitals with high patient turnover.
Key Features of Beata Clasp
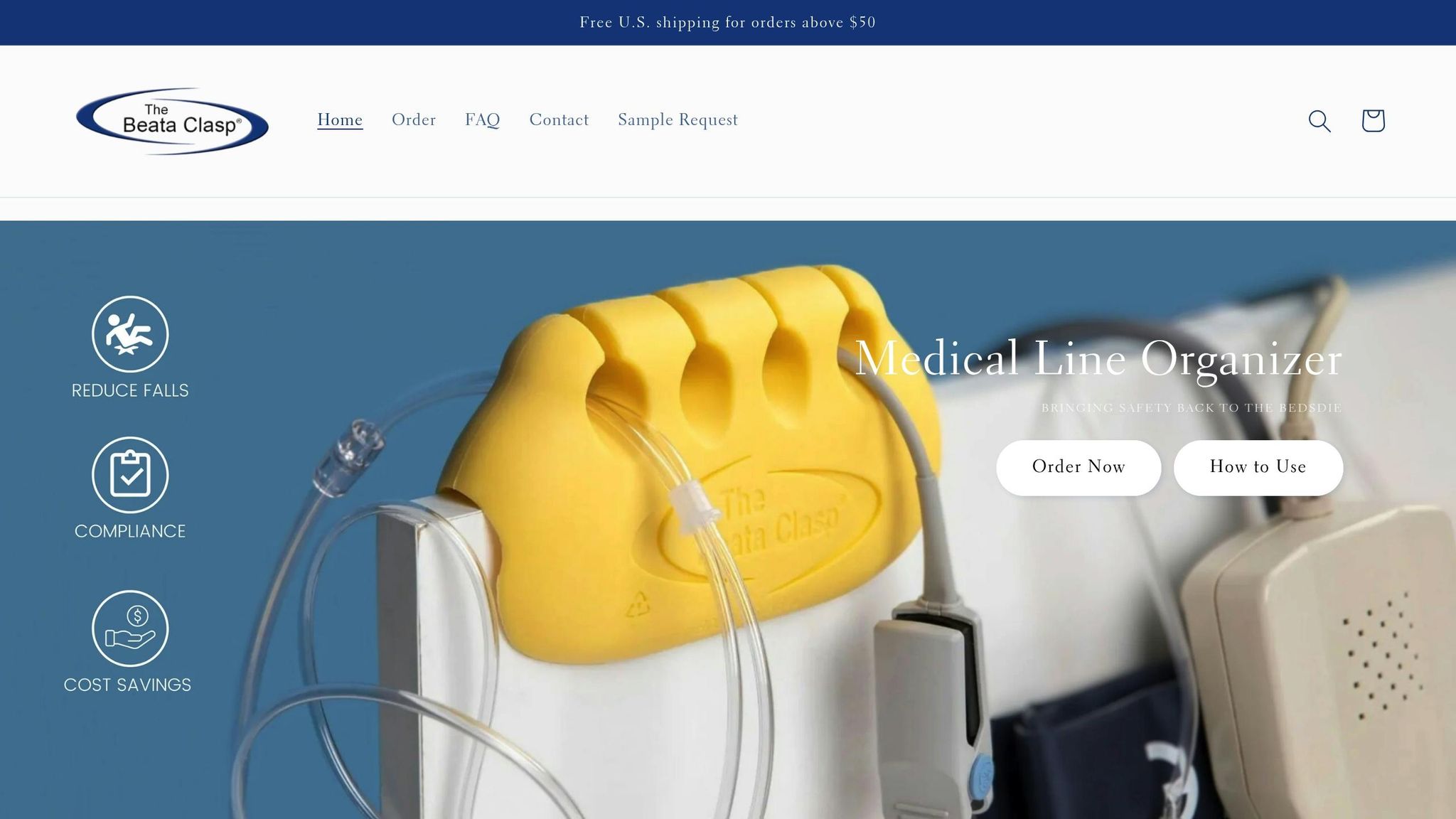
One standout example of innovation in this space is the Beata Clasp. This soft foam organizer is designed to securely attach to hospital bedrails, offering a compact and effective way to manage multiple IV lines.
Some of its standout features include:
- Antimicrobial finish to inhibit bacterial growth
- Latex-free material for allergy-safe use
- Circular groove design that prevents kinks, dislodging, and tangles
- Easy-to-clean recyclable foam to support infection control efforts
- Versatile use for hospitals, ICUs, and even home care settings
The Beata Clasp’s design ensures that each line stays in its proper place and maintains the correct flow rate, reducing the risk of disruptions in medication delivery. Healthcare workers have noted that using the Beata Clasp cuts down on tangling, saves time at the bedside, and lowers frustration. These benefits not only improve patient care but also contribute to better job satisfaction for medical staff.
Conclusion: Better Patient Safety Through Proper IV Line Management
Handling multiple IV lines effectively is critical for ensuring patient safety. Consider this: research shows that up to 50% of IV lines fail before they are removed. This statistic highlights the importance of having solid management systems in place.
Back in 2017, the World Health Organization introduced the 3rd Global Patient Safety Challenge - Medication Without Harm. The goal? To cut serious and preventable medication-related harm by half by 2022. Reaching such an ambitious target requires tackling the root causes of IV line complications with systematic and well-coordinated strategies.
These global efforts emphasize the importance of unified clinical practices. To achieve the best outcomes in IV therapy, healthcare teams must work together. This includes timely IV insertion, consistent monitoring, removing unnecessary lines promptly, and addressing complications as soon as they arise.
Nearly half of adverse drug events could be avoided with better administration practices, which underscores the need for practical solutions. For example, recent studies point to the benefits of incorporating IV line organizers into care routines. In a simulated ICU study involving 40 nurses, the use of line labels and organizers completely eliminated infusion identification errors (0% error rate compared to 7.7% without these tools). Nurses using these aids also worked faster, identifying infusions in just 31 seconds versus 1 minute and 20 seconds without them.
Healthcare facilities have access to practical tools to improve safety. Take the Beata Clasp, an IV line organizer priced at $19.95 per unit. This antimicrobial, latex-free device helps reduce risks like line entanglement, contamination, and even patient falls. For those hesitant to commit, evaluation packs provide a budget-friendly way to test its effectiveness.
Looking ahead, standardizing labels and incorporating IV line organizers into protocols can serve as a cornerstone for safer and more efficient multi-line therapy.
FAQs
How does the Beata Clasp help prevent medication errors when managing multiple IV lines?
The Beata Clasp is designed to minimize medication errors in setups with multiple IV lines. It keeps the lines neatly organized, clearly labeled, and properly separated. This structured approach allows healthcare professionals to identify the right line quickly, reducing the chances of mix-ups or administering the wrong medication.
In fast-paced settings like ICUs or hospitals, where multiple IV lines are often used, the Beata Clasp simplifies the process. It not only saves time but also plays a vital role in maintaining patient safety.
How can healthcare professionals maintain proper hygiene and prevent infections when managing multiple IV lines?
To keep things clean and reduce the risk of infections when dealing with multiple IV lines, always prioritize proper hand hygiene. This means washing your hands thoroughly with soap and water or using an alcohol-based hand sanitizer before touching any IV lines. Use aseptic techniques during both insertion and handling to avoid contamination. For skin preparation, applying a chlorhexidine solution with alcohol is one of the most effective methods to cut down infection risks.
Make sure IV dressings stay clean, dry, and secure. If there's any oozing at the site, gauze dressings are a better choice. It's also critical to stick to sterile precautions, like keeping the IV system closed and using sterile barriers during insertion. By consistently following these steps, you can greatly reduce the chances of infections and other complications.
Why is it important to standardize IV line labeling, and how does it enhance patient safety?
Clear and consistent labeling of IV lines is crucial for reducing medication errors and ensuring patient safety. When labels are standardized, healthcare providers can quickly and accurately identify IV lines, which is especially important when dealing with high-risk medications or managing multiple lines. This minimizes confusion and helps prevent dangerous mix-ups.
Standardized labels also help streamline workflows, making it easier for teams to follow safety protocols and communicate effectively. This not only supports better care delivery but also creates a safer environment for patients.
