Every day, U.S. hospitals insert 410,000 peripheral IV catheters, essential for delivering medication and fluids. But these routine procedures carry significant risks, including medication errors, infections, and catheter failures. Poor IV line management leads to longer hospital stays, higher costs, and severe patient complications. For example:
- 56% of medication errors involve IV drugs, with 38% occurring during administration.
- IV complications can extend hospital stays by 2 days and increase costs by $4,000 per patient.
- 46% of IV lines fail before their intended lifespan, causing disruptions in treatment.
The solution lies in evidence-based protocols, regular safety checks, and tools like the Beata Clasp, which organizes IV lines to reduce errors and contamination. Hospitals adopting these practices report fewer complications, shorter patient stays, and significant cost savings. Proper IV line management isn’t just about avoiding harm - it’s about creating safer, more efficient care for everyone involved.
How To Maintain An IV Line? - Nursing Knowledge Exchange
Risks of Poor IV Line Management
Managing IV lines might seem routine, but the risks tied to poor management are far from trivial. What starts as a minor issue can quickly spiral into a life-threatening situation. Understanding these risks is a key step toward safer practices.
Common IV Line Complications
One of the most frequent issues is infiltration, which affects about 24% of peripheral IV lines on average. This happens when the catheter punctures the vein wall, causing medication to leak into nearby tissues. While it might start with mild swelling, it can escalate to serious tissue damage, especially when harsh medications are involved.
Phlebitis, another common problem, occurs in 15% of peripheral IVs. This condition involves vein irritation, often caused by the catheter’s movement or a reaction to medication. Symptoms include pain, redness, and swelling along the vein. If left untreated, it can lead to more severe infections.
Occlusion is when biological material clogs the IV catheter, leading to a blockage. It accounts for 19% of IV catheter failures. A blocked catheter can delay critical medications and fluids, often requiring a painful reinsertion.
Dislodgement affects 7% of IV lines. This happens when mechanical forces, like patient movement or inadequate securement, cause the catheter to shift or come loose. Dislodged IV lines interrupt treatments and increase contamination risks.
Overall, IV failures occur in 46% of cases at major clinical centers before the catheter reaches its intended lifespan. Additionally, more than half of patients experience local complications at the IV access site.
What Causes IV Line-Related Harm
Several factors contribute to IV line complications. Mechanical issues, like patient movement or tangled tubing, can cause the catheter to shift, leading to problems such as irritation, infiltration, or dislodgement.
Infection control lapses are another significant contributor. Poor hand hygiene, inadequate skin antisepsis, and contaminated equipment can introduce harmful microbes. Studies reveal that 33–45% of needleless connectors are contaminated, with disinfection compliance as low as 10%.
Improper stabilization of the catheter is also a concern. When stabilization is inadequate, even slight movements can allow microorganisms to migrate, increasing the risk of bloodstream infections. On top of that, insufficient training among healthcare workers can lead to poor aseptic techniques, improper site selection, or a failure to catch early warning signs of complications.
Systemic issues, like inconsistent labeling, infrequent site inspections, and delays in catheter replacement, can allow minor problems to go unnoticed until they escalate. Addressing these gaps is crucial for improving patient safety.
Effects on Patient Health and Healthcare Costs
The impact of poor IV line management goes beyond patient discomfort - it can lead to serious health outcomes and higher healthcare costs. For instance, IV complications can extend hospital stays by an average of 2 days (5.9 days compared to 3.9 days) and increase costs by over $3,000.
Patients with IV complications are also twice as likely to require intensive care (20.4% versus 11.0%), and their risk of dying during hospitalization nearly triples (3.6% versus 0.7%).
Even after discharge, the effects linger. Patients who experience complications are less likely to return home (62.4% versus 77.6%) and often need extended care or rehabilitation services. These statistics highlight the pressing need for effective IV line management to protect patients and reduce healthcare costs.
Key Methods for Safe IV Line Management
Effective IV line management hinges on following established protocols and equipping nurses with the tools and knowledge they need to deliver safe and efficient care. These strategies not only improve patient outcomes but also help control healthcare costs.
Using Proven Protocols
The backbone of safe IV line practices lies in evidence-based protocols that address every step of catheter care. For instance, assessing the catheter insertion site daily allows healthcare providers to spot and address complications early. Simple measures like proper hand hygiene before handling catheters and maintaining aseptic techniques during catheter use significantly reduce infection risks.
Central venous catheter (CVC) insertion benefits greatly from maximal sterile barrier precautions - this means using sterile gloves, gowns, masks, and large sterile drapes. Additionally, chlorhexidine-based antiseptics are shown to lower infection risks by 49% compared to povidone iodine when preparing the skin.
Specialized IV teams have demonstrated success in lowering catheter-related bloodstream infections and associated complications. For example, the Cleveland Clinic reported that nearly 58% of successful IV placements utilized ultrasound guidance, underscoring the role of advanced techniques in improving outcomes.
These protocols establish a solid framework for consistent and safe IV line management, which is further reinforced by standardized procedures.
Standard Procedures for IV Line Safety
Consistency is critical in ensuring IV line safety. Proper labeling and careful line tracing help ensure medications are delivered to the right patient, reducing the risk of potentially dangerous errors.
Catheter selection is another key area. Choosing the right device - based on its intended use and duration - minimizes vein trauma. Using the smallest gauge catheter suitable for the therapy can also reduce complications. For adults, upper extremity sites are generally preferred for catheter placement, while femoral veins are avoided due to a higher risk of infection.
Securement methods, like sutureless securement devices, offer another layer of protection. These devices lower infection risks compared to traditional sutures and help keep the catheter and tubing in place, preventing accidental dislodgement.
Clear and thorough documentation is essential for maintaining accountability and ensuring continuity of care. Recording details such as insertion procedures, site assessments, and any complications not only enhances patient safety but also reduces potential legal risks.
Protocols for rotating and replacing catheters are equally important. Peripheral venous catheters should be removed immediately if there are signs of phlebitis or infection, while central lines should be discontinued as soon as they are no longer necessary.
With these procedures in place, the focus shifts to empowering the nurses who bring these protocols to life.
How Nurses Drive IV Line Safety
Nurses are at the forefront of IV line safety, and their role is pivotal in ensuring the success of established protocols. By combining standardized procedures with their clinical expertise, nurses adapt strategies to meet the unique needs of their patients. Regular education and skills assessments are vital for maintaining high standards in IV catheter insertion and care.
"Empowering Nurses is the concept that increasing the authority or power nurses have through innovation, education, and training, will create more efficient and effective healthcare in all healthcare settings." – Vascular Wellness
Nurse-led vascular access teams (VATs) are a prime example of how nurses can enhance IV line safety. These teams streamline processes and improve patient care. Annual competency assessments ensure all staff involved in IV therapy are up to date with the latest practices. According to the American Nurse Association, trained nurses using ultrasound-guided insertion can reduce the need for central venous catheters by as much as 80%.
Patient education is another area where nurses make a significant impact. By teaching patients to recognize signs of complications, nurses empower them to take an active role in their care and report issues early.
On the front lines, nurses often develop practical solutions to everyday challenges. As Dr. Oleg Zaslavsky, Director of DHIH, noted, these innovations represent "pragmatic, nurse-informed solutions to an everyday safety issue that nurses have silently struggled with for decades".
Step-by-Step Guide for Routine IV Line Safety Checks
Routine assessments of IV lines are crucial for identifying potential risks and ensuring patient safety. These checks should be part of every interaction with a patient, seamlessly integrated into your daily routine. By making these evaluations a natural part of your workflow, you not only enhance safety but also improve accuracy in line tracing and documentation.
Checking Insertion Sites by Sight and Touch
Take a close look at the IV insertion site for any signs of redness, swelling, tenderness, coolness, or warmth. Gently feel over the dressing to check for discomfort that might not have been reported. Encourage patients to alert you if they notice tenderness or swelling at the site.
For example, a neonatal intensive care unit that implemented evidence-based guidelines, including better surveillance and staff training, saw an increase in reported IV complications from five to nine per 1,000 line days. While this might seem concerning, it actually reflected improved detection of issues. At the same time, severe Stage 4 infiltrates significantly decreased during the same period.
Be vigilant for signs of infection, such as pain, redness, swelling, crusting, scabbing, or oozing. Peripheral vascular catheters are among the most commonly used invasive devices in hospitals, with 30–80% of patients requiring at least one during their stay.
"IV lines are useful but can cause problems. They can become blocked, leak fluid into the skin and cause infection." - HSE.ie
Following IV Lines from Bag to Patient
Always trace the IV line from the fluid bag, through any pumps, and all the way to the patient. This helps you spot kinks, disconnections, or irregularities. Before accessing a port, clean the catheter cap with an alcohol pad for at least five seconds and let it dry completely.
"As part of your head-to-toe assessment and room safety check, you want to always trace your lines... bag, pump, patient." - Straight A Nursing
Pay extra attention to setups with multiple lines. Clear identification and secure placement are essential to prevent mix-ups or accidental disconnections. A thorough visual inspection naturally leads to the next step: proper labeling and record keeping.
Proper Labeling and Record Keeping
Labeling IV lines correctly is critical. Include details such as the medication or fluid name, concentration, dose, preparation time, change date/time, and the initials of the staff member who prepared it. Place labels near the port or Y-site closest to the patient and ensure they remain visible during care activities.
Improper labeling is a significant safety risk, with medication errors occurring in as many as 1 in 5 doses in U.S. hospitals. Accurate labeling helps reduce these risks, especially when dealing with high-alert medications, which are involved in 71% of multiple IV infusion errors and 92% of IV line mix-ups. Use medication flags to identify these drugs and apply reminder labels for tubing changes.
Additionally, include IV fluids in the patient’s input/output records to maintain precise fluid balance. Considering that up to 80% of hospitalized patients receive IV treatment during their stay, consistent labeling and documentation are vital for ensuring safety across all levels of care.
sbb-itb-f779e18
Tools and Products for IV Line Safety
Having the right tools on hand can transform IV line management from a potential source of chaos into a streamlined and safe process. To tackle challenges like contamination risks, tangled lines, and inefficient workflows, healthcare facilities are increasingly adopting specialized solutions. Among these, tools like the Beata Clasp stand out for their ability to enhance safety and organization.
The Beata Clasp: Features and Benefits
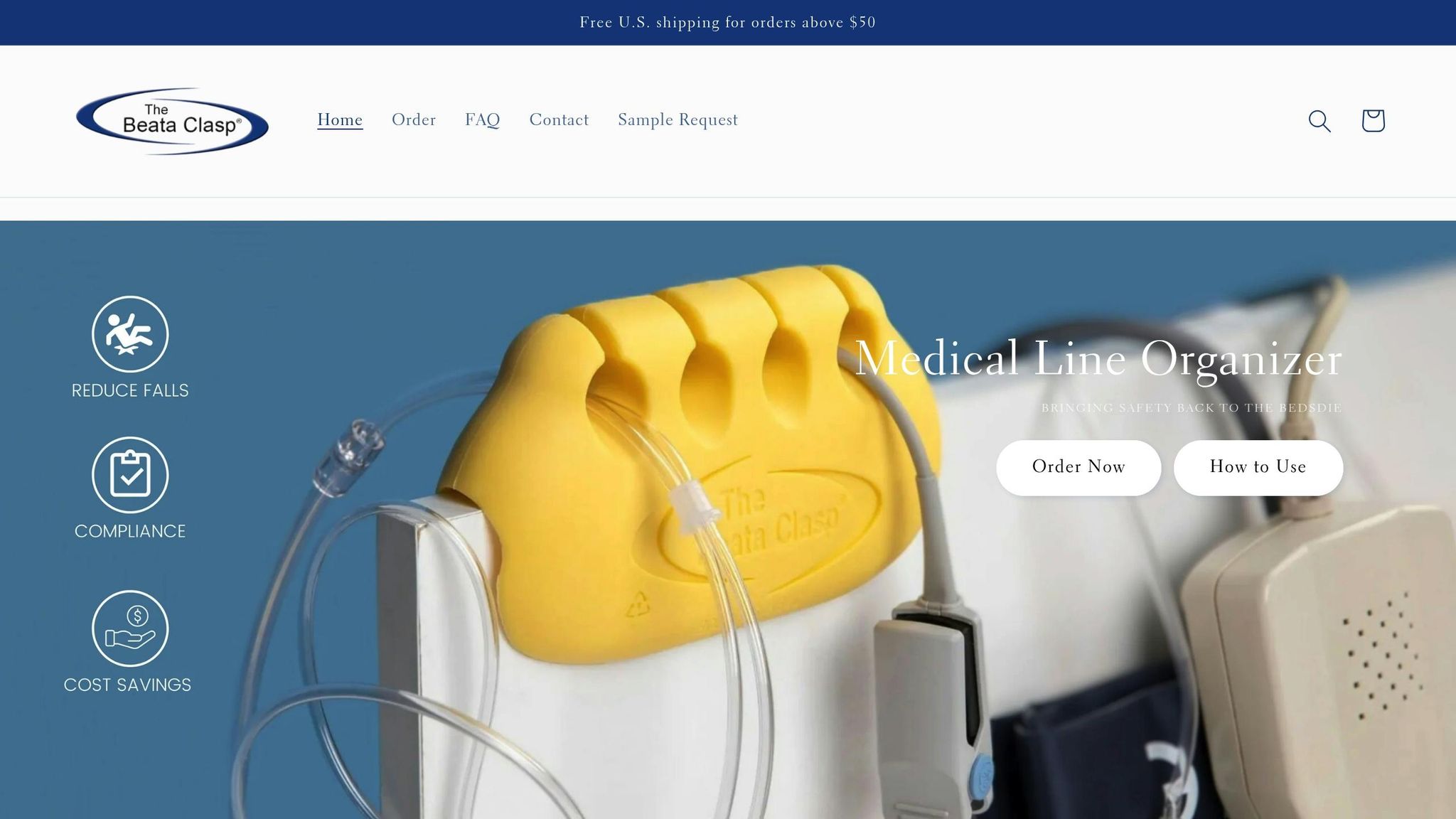
The Beata Clasp is a medical line organizer specifically designed to simplify IV line management. Created by experienced registered nurses, it addresses several common safety issues in one compact device.
- Antimicrobial Protection: This feature helps reduce contamination risks, a critical consideration in infection control.
- Latex-Free Design: Ideal for patients with allergies, ensuring broader compatibility.
- Eco-Friendly Materials: Made from recyclable components, the clasp supports sustainability efforts.
- No Adhesives: Eliminates sticky residues and minimizes the risk of skin irritation often caused by tape-based solutions.
- High-Alert Color: Bright coloring ensures quick and easy line identification.
- Elevated Line Design: Keeps IV lines off surfaces, reducing contamination risks and preventing disconnection during patient movement.
The Beata Clasp is versatile enough for single or multiple IV lines and can be introduced as soon as a patient requires a second line. This early intervention helps maintain order and clarity throughout treatment.
Advantages of Dedicated Line Organizers
Dedicated line organizers are more than just accessories - they’re essential tools for maintaining patient safety. They complement routine safety checks by simplifying line tracking and reducing the chance of mix-ups. Organized lines make it easier for healthcare providers to trace tubing from the source to the patient, improving efficiency and accuracy in care.
By keeping tubing elevated and away from high-traffic areas, these organizers also reduce the risk of falls and contamination. This supports compliance with infection control guidelines from organizations like the CDC and WHO. In emergencies, clear and orderly line management can save valuable time.
Comparing IV Line Management Methods
Here’s a quick look at how different IV line management methods stack up in terms of benefits, drawbacks, and costs:
| Method | Benefits | Limitations | Cost Considerations |
|---|---|---|---|
| Tape/Adhesive Solutions | Affordable, widely available | Can irritate skin, leaves residue, temporary hold | Ongoing replacement costs |
| Clip-on Organizers | Reusable, no adhesives, easy to clean | May not fit all bed types, limited capacity | Higher upfront cost, lower long-term expense |
| Built-in Bed Features | Integrated and permanent | Expensive to retrofit, lacks flexibility | High initial investment |
| Beata Clasp | Antimicrobial, portable, no training needed | Requires initial purchase | $19.95 per unit, bulk discounts available |
The Beata Clasp stands out for its combination of safety, convenience, and cost-effectiveness. Unlike tape-based solutions, it’s reusable and doesn’t leave sticky residue. Unlike built-in bed features, it’s portable and works seamlessly with existing equipment, avoiding the need for costly modifications. Additionally, its antimicrobial properties and high-alert color offer significant advantages over traditional methods.
For facilities exploring options, the Beata Clasp is available in various purchasing formats: individual units for $19.95, evaluation packs (10 units) for $163.00, and bulk orders (25 units) for $467.50. This tool aligns with broader strategies for improving IV therapy safety, such as staff training and the use of health IT systems. With IV failure rates and complications affecting up to 53% of cases, incorporating reliable tools like the Beata Clasp is a practical step toward better patient outcomes and cost savings.
Proven Methods and Success Examples
These examples highlight a powerful truth: effective IV line management turns potential risks into safe, everyday practices. By blending multiple strategies, healthcare facilities have seen measurable improvements in IV line safety. The success stories below illustrate how a structured approach can significantly reduce patient harm and enhance outcomes.
Combining Safety Measures for Better Outcomes
When it comes to IV line safety, using multiple strategies together yields the best results. Regular safety checks, clear labeling, specialized tools, and consistent staff training all work in tandem to lower complications.
Take the example of a tertiary care hospital in North India. Between June and September 2017, the pediatric emergency department launched a quality improvement initiative. They introduced innovative tray systems, conducted regular audits, made organizational changes, and emphasized infection control. The results were striking: infiltration rates dropped from 82.9% to 45%, and phlebitis cases fell from 96.1% to 55%.
Another breakthrough came with illuminated smart-lite technology, which simplifies medication line identification. At Wake Forest University School of Medicine, nurses using smart-lite systems identified primary medication lines 24% faster than traditional methods. This approach also reduced cognitive strain by 40% and eliminated errors in darkened room conditions. Similarly, at a U.S. Veterans Affairs Hospital in Houston, Texas, a four-month study showed that smart-lite systems cut injection readiness time by over 400%, reducing administration time from up to 58 seconds to just 1 second. These examples show how combining tools, training, and protocols can streamline workflows and improve safety.
Workflow and Safety Improvements in Action
Building on integrated safety protocols, process improvements can further boost efficiency and safety. For instance, one emergency department applied Lean principles, such as visual management systems, standardized workflows, and organized supply management, reducing patient wait times by 45%. Systematic improvements have also led to 20–30% increases in operational efficiency, 50–70% reductions in medication errors, and a 40% drop in hospital-acquired infections.
Color-coded safety systems have proven effective in minimizing medication errors as well. These systems not only speed up medication administration but also help prevent wrong-route errors - responsible for 15% of all infusion-related adverse drug events.
Additionally, tools designed by nurses to reduce line entanglement have made workflow smoother and more organized. Facilities report that these improvements allow nurses to spend more time on direct patient care.
"The Beata Clasp is more than a product - it's a movement toward clarity, visibility, and the kind of care every patient deserves." - BeataClasp
Comprehensive line management programs that integrate standardized protocols, staff training, and the right tools not only improve patient safety but also cut costs. For example, such programs can save around $450,000 annually in avoidable direct adverse drug event costs per 100 beds.
The takeaway? IV line safety requires a systematic approach. While individual strategies offer value, the most dramatic improvements come from combining proven methods with ongoing staff support and quality monitoring.
Conclusion: Making Safety a Daily Practice
Turning IV line management into a seamless part of daily routines requires commitment, vigilance, and the right tools. When healthcare providers make safety checks a regular part of their workflow, patient outcomes improve, and costs decrease.
Nurses play a key role in this process by routinely inspecting IV sites for redness, swelling, or tenderness, tracing tubing back to its origin, and ensuring IV line patency by checking for blood return and proper flushing. Following standardized protocols and maintaining thorough documentation - aligned with USP <797> regulations - help reinforce these critical practices.
Patient involvement adds another layer of protection. Educating patients about the importance of reporting any discomfort or irritation at IV sites turns them into active participants in their own care. Additionally, vascular access teams conducting daily rounds further enhance safety measures.
Managing IV lines proactively leads to better outcomes and significant cost savings. IV complications impact up to 53% of patients, often extending hospital stays from under four days to six days and increasing average hospital costs from $7,000 to nearly $11,000. Preventing these complications can also dramatically lower mortality rates, reducing the risk of death from 3.6% to 0.7%. These measures not only benefit patients but also strengthen the financial health of healthcare institutions.
Tools like the Beata Clasp support these efforts by maintaining IV line organization and keeping lines off the floor. With antimicrobial properties and a high-alert color design, it addresses risks such as patient falls, which are a major concern in hospitals and can cost over $36,000 per incident.
Making IV line safety a daily habit means consistently applying aseptic techniques, adhering to tubing change protocols, and keeping detailed records. When safety becomes as routine as checking vital signs, the quality of patient care improves significantly. With the right mix of awareness, protocols, and tools, healthcare providers can work toward the ultimate goal: eliminating preventable harm in IV line management.
FAQs
What are the most common risks of peripheral IV catheters, and how can they be avoided?
Peripheral IV catheters can sometimes lead to issues like infiltration, phlebitis, occlusion, infection, and extravasation. However, healthcare professionals can greatly minimize these risks by adopting a few essential practices:
- Selecting the most appropriate insertion site based on the patient's needs
- Applying strict aseptic techniques during insertion
- Properly securing the catheter to limit unnecessary movement
- Keeping a close eye on the site for any signs of complications
- Removing the catheter as soon as it’s no longer required
By consistently following these steps, medical teams can enhance patient safety and reduce the chances of complications.
How does the Beata Clasp enhance IV line management and help prevent complications?
The Beata Clasp simplifies managing IV lines by keeping them neat, preventing tangles, and minimizing contamination risks. It ensures lines remain off the floor, contributing to a cleaner and safer space for both patients and healthcare staff.
By keeping lines stable and organized, the Beata Clasp reduces the likelihood of issues like infections, misconnections, or accidental trips. Its thoughtful design also prioritizes patient mobility, making it easier for individuals to move around safely and comfortably.
What is the role of nurses in maintaining IV line safety, and what training or tools help them perform this effectively?
Nurses play a key role in ensuring IV line safety by closely monitoring insertion sites, maintaining proper care routines, and following strict infection control measures. Their attention to detail helps minimize risks such as infections, blockages, or accidental dislodgement of the line.
To carry out these responsibilities effectively, nurses require thorough training in sterile techniques, IV insertion, and ongoing maintenance. This training is often delivered through hands-on workshops, realistic simulations, or certification programs like VA-C or CRNI. They also rely on vital tools such as sterile supplies, infusion pumps, and safety checklists to provide consistent, high-quality care while safeguarding patients against potential complications.
