Nurses face frequent interruptions, especially during IV line tasks, which directly impact patient safety and efficiency. Key findings include:
- Nurses are interrupted 10.5-13 times per hour, with over 50% of medication administrations disrupted at least once.
- Each interruption increases procedural failures by 12.1% and clinical errors by 12.7%.
- Interrupted tasks take 19% longer to complete compared to uninterrupted ones.
- IV push procedures are interrupted 100% of the time, often multiple times, raising the risk of errors.
- Common interruption sources include face-to-face requests (58.7%), self-initiated tasks (20.7%), and alarms (3.7%).
Interruptions also lead to delays, contamination risks, and adverse events like IV dislodgements, which cost the U.S. healthcare system $2 billion annually. Solutions include creating no-interruption zones, addressing workflow inefficiencies, and using tools like the Beata Clasp to organize IV lines and reduce alarm-related disruptions.
Reducing interruptions is critical to improving nurse efficiency and patient safety.
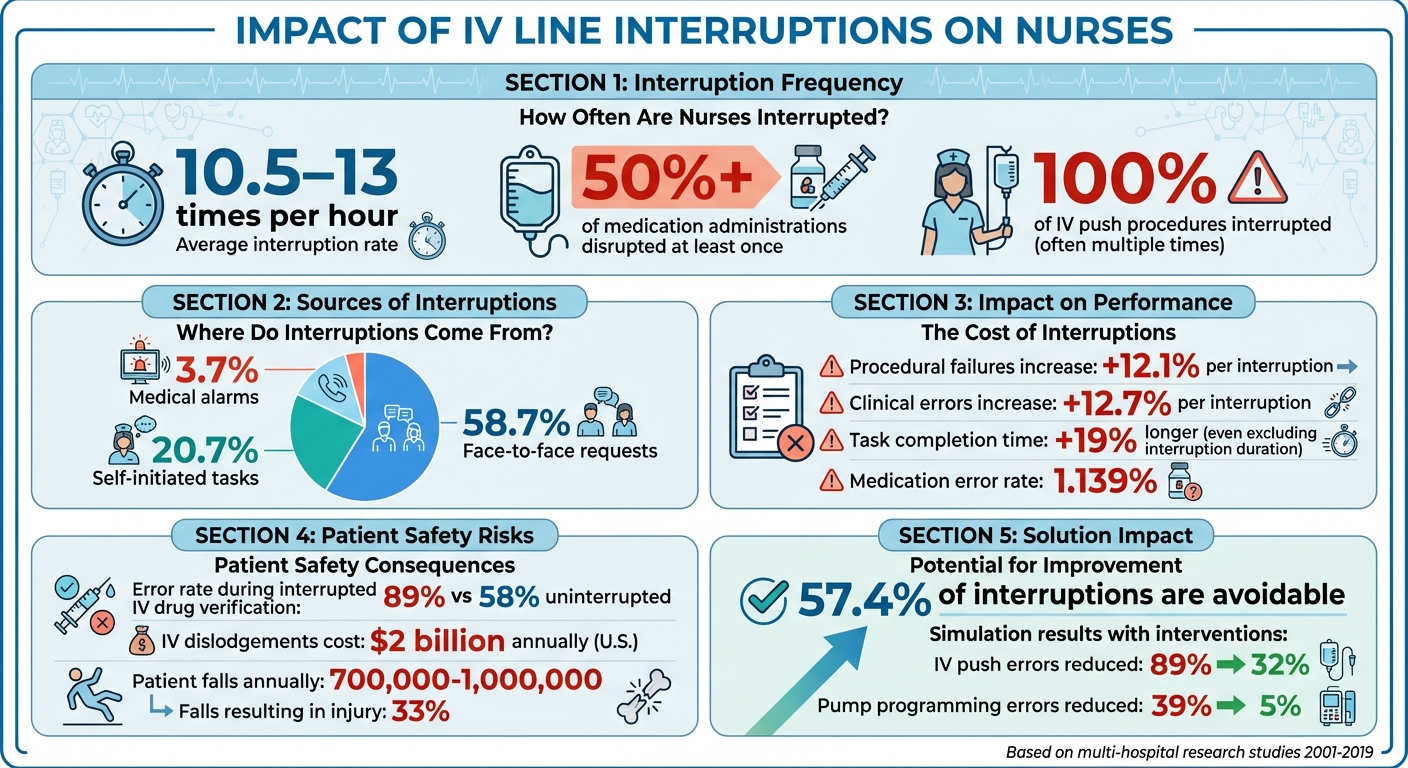
Impact of IV Line Interruptions on Nurses: Key Statistics and Patient Safety Risks
Red Zone Medication Safety Initiative by J. Dwyer, B. Small, R. Brediger | OPENPediatrics
Study Overview: How IV Line Interruptions Affect Nurses
This study takes a closer look at how interruptions during IV line management impact nurses, using detailed observations and simulations to quantify the effects.
Research Design and Methods
Researchers employed several methods to track and measure nursing interruptions. Direct observation was a key approach, with nurses being monitored using stopwatches to record the frequency, source, and duration of each disruption. Between September 2018 and February 2019, Wei Wang, Lin Jin, and Xu Zhao observed 270 hours of nursing work across four cardiology wards at Shandong Provincial Hospital. During this time, 3,424 interruptions were documented, averaging 12.68 interruptions per hour. These interruptions consumed 9.87% of the total observation time (equivalent to 26.65 hours) and were linked to a medication error rate of 1.139%.
In addition to direct observation, simulated scenarios were used to assess the impact of interruptions on IV push performance. By comparing error rates in interrupted versus uninterrupted environments, researchers isolated the specific effects of disruptions. For example, in 2001, Anita L. Tucker studied 11 nurses over full shifts (averaging 9 hours and 51 minutes each) at six U.S. hospitals. Her field journal entries revealed that nurses faced an average of 8.4 work system failures per 8-hour shift, with tasks often lasting only 3.1 minutes due to frequent interruptions.
Patient Safety Event (PSE) reports from hospital databases were also analyzed. Researchers used keyword searches and manual reviews to identify outcomes linked to interruptions. To complement this quantitative data, qualitative methods such as focus groups and semi-structured interviews captured nurses' firsthand accounts of how interruptions, described as "hassles" and "glitches", increased their cognitive workload.
Main Research Question
The central question driving this study was: How do IV line interruptions affect nursing efficiency and patient safety? Researchers explored whether interruptions led to higher error rates, longer task completion times, and delays in care for multiple patients. Professor Westbrook from the Australian Institute of Health Innovation highlighted the risks, stating:
"Each interruption was associated with a 12.1% increase in procedural failures and a 12.7% increase in clinical errors."
Tara McCurdie from the Techna Institute further emphasized the findings:
"The percentage of nurses who made errors when performing IV pushes during simulated scenarios was significantly higher when interrupted than in the uninterrupted condition."
The study also delved into the primary sources of interruptions. In China, family members were the most common cause, while in the U.S., interruptions were primarily caused by other nursing staff. Researchers found that 58.7% of interruptions came from face-to-face requests, followed by self-initiated interruptions (20.7%), phone calls (11.1%), and medical alarms (3.7%). These findings highlight the varied origins of disruptions and their role in compromising patient safety.
Key Findings: How Interruptions Impact Nursing Work
Performance and Time Results
Interruptions have a noticeable impact on nursing efficiency. On average, interrupted tasks take 682.02 seconds to complete, compared to just 296.47 seconds for uninterrupted ones. Even when the time of the interruption itself is excluded, tasks still take an additional 121.36 seconds, representing a 19% increase in duration. Gai Cole from Emergency Medicine at Johns Hopkins Medicine highlighted this issue:
"Interrupted interventions were 121.36 s... longer, a 19 percentage point increase... than an intervention without (excluding the length of the interruption)".
IV push administration is particularly affected, with nurses being interrupted 100% of the time during these procedures - often multiple times. These interruptions disrupt the precise timing required for IV push delivery, increasing the risk of adverse complications.
| Nursing Intervention Status | Average Duration (Seconds) | Median Duration (Seconds) |
|---|---|---|
| Uninterrupted | 296.47 | 185.15 |
| Interrupted (Total Time) | 682.02 | 589.63 |
These extended durations not only slow individual tasks but also exacerbate broader challenges within nursing workflows.
Workflow Disruptions
Interruptions don’t just increase task times - they also disrupt workflows, particularly during medication administration. Over 50% of all medication administrations encounter interruptions. Within this workflow, the administration phase accounts for 24.1% of interruption-related safety events, while the ordering phase contributes 16.8%. Laboratory processes are also impacted, with 22.7% of interruption-related errors occurring during lab work - 75% of these errors involve specimen mislabeling.
The fragmented nature of nursing tasks compounds these issues. On average, tasks last just 3.1 minutes, and nurses shift between patients roughly every 11 minutes. Additionally, nurses face an average of 8.4 operational failures per 8-hour shift, such as missing medications or malfunctioning equipment. These failures consume about 42 minutes per shift as nurses work to resolve them. Kalila Marple, an oncology nurse, described the ripple effect of these challenges:
"Sometimes it [an operational failure] has a snowball affect that if you face a huge obstacle in one area with one of your patients, the next thing you know the next patient is paying for that extra time that you had to keep shifting back".
These disruptions not only affect individual tasks but also create a cascading impact on patient care and overall workflow efficiency.
Patient Safety Risks from Interruptions
Medical Errors and Treatment Delays
Interruptions during medical procedures don’t just slow things down - they can seriously compromise patient safety by increasing the likelihood of errors. For instance, in simulated scenarios, nurses faced an alarming 89% error rate when verifying syringe drug volumes while being interrupted, compared to 58% when working without interruptions. Errors during intravenous (IV) drug administration are particularly concerning, as they’re five times more likely to occur than with other methods.
Interruptions also disrupt cognitive focus, making it easier to miss critical steps or make clinical mistakes. This is especially dangerous during IV push administration, where distractions can lead to doses being delivered too quickly or too slowly, potentially causing harmful drug reactions. When interruptions happen repeatedly, the risks compound, further threatening patient care.
But the dangers don’t stop at performance errors - interruptions can also lead to physical harm.
Contamination and Fall Risks
Interruptions create physical hazards that go beyond clinical mistakes. Mismanaged IV lines during interruptions pose serious risks, including contamination and dislodgement. In fact, IV line dislodgements cost the U.S. healthcare system around $2 billion annually. A survey of 1,500 doctors revealed that 58% witnessed daily IV dislodgements, and over 90% saw them at least weekly. Dislodged or improperly secured IV lines increase the risk of contamination and can lead to dangerous complications.
Take, for example, a case reported by PSNet in September 2012. A 75-year-old man with congestive heart failure had a peripheral IV left in place beyond the recommended four days. By day six, the patient developed cellulitis at the IV site, which escalated into MRSA bacteremia and a spinal epidural abscess. Treating these complications required six weeks of IV antibiotics, a prolonged hospital stay, and significant financial costs.
IV lines also contribute to a staggering number of patient falls - between 700,000 and 1,000,000 annually in U.S. hospitals. Roughly 33% of these falls result in injuries such as fractures or internal bleeding, with serious cases leading to hospital charges exceeding $4,200 per patient. Patients sometimes use IV poles for support or trip over unsecured tubing, further increasing their risk. Dr. Ryan Dennis, CEO of Linear Health Sciences, shared an incident where a patient dislodged a chest tube just 10 minutes after falling asleep by rolling over. The dislodgement caused the patient’s lung to collapse, requiring emergency surgery to replace the tube.
These examples highlight how interruptions can have far-reaching consequences, both in terms of patient safety and healthcare costs.
sbb-itb-f779e18
How to Reduce IV Line Interruptions
Creating No-Interruption Zones
Interruptions during critical nursing tasks, especially medication-related ones, can have serious consequences. Studies show that medication tasks are disrupted 50.9% of the time, with the most vulnerable phases being administration (24.1%) and ordering (16.8%). Each interruption raises the likelihood of procedural failures by 12.1% and clinical errors by 12.7%. This highlights the importance of establishing "no-interruption zones" during these high-risk moments.
Operational failures - such as missing medications, broken equipment, or unavailable supplies - are another major source of interruptions. Nurses encounter an average of 8.4 operational failures during an 8-hour shift, forcing them to stop and resolve these issues. Tackling these inefficiencies can free up valuable time and minimize unnecessary disruptions.
"Our findings suggest that nurse effectiveness can be increased by creating improvement processes triggered by the occurrence of work system failures, with the goal of reducing future occurrences. Second, given that nursing work is fragmented and unpredictable, designing processes that are robust to interruption can help prevent errors." - Anita L Tucker, D.B.A., M.S., The Wharton School
While some interruptions, like those caused by urgent patient needs, are unavoidable, nursing workflows should be designed to handle disruptions safely. Processes that allow nurses to resume tasks seamlessly after an interruption can significantly reduce errors. Alongside these process changes, specialized tools can also play a key role in reducing IV line interruptions.
Using Tools Like BeataClasp
Specialized tools, such as the Beata Clasp, can help organize IV lines and reduce interruptions caused by operational alarms. Research indicates that 28.7% of unique infusions experience at least one operational alarm, with tubing kinks being a major contributor to both downstream and upstream occlusion alarms. These alarms interrupt medication delivery and require manual intervention, pulling nurses away from other critical tasks.
The Beata Clasp addresses these issues by preventing line entanglement and false alarms. Its design keeps tubing off the floor, reducing the risk of contamination, falls, and infections. Key features include an antimicrobial, latex-free build, a high-alert color for visibility, and an easy-to-clean surface. It also avoids adhesives, making it suitable for single-patient and multi-patient use in hospitals, ICUs, and home care settings. Priced at $19.95 per unit or $467.50 for a pack of 25, it offers a practical and affordable solution for healthcare providers.
What This Means for Nursing Practice
The documented impact of IV interruptions on both workflow and safety sheds light on critical implications for daily nursing practice. As outlined earlier, interruptions in IV line management significantly raise the risk of errors, affecting patient outcomes and nursing efficiency. For instance, nurses encounter interruptions during 50% of safety events and nearly 51% of medication tasks, with each interruption increasing procedural failures by 12.1% and clinical errors by 12.7%.
Comparison of Outcomes
Interruptions create striking differences in nursing workflows, as seen in measurable outcomes:
| Outcome Metric | Uninterrupted Condition | Interrupted Condition |
|---|---|---|
| Procedural Failure Rate | 70% baseline | Increases by 12.1% per interruption |
| Clinical Error Rate | 25% baseline | Increases by 12.7% per interruption |
| IV Push Accuracy | Higher adherence to recommended speeds | More frequent deviations from recommended speeds |
| Error Severity | Lower baseline severity | Severity increases with interruption frequency |
| Lab Specimen Accuracy | Standard protocol adherence | 75% of lab-related errors result in mislabeling |
These figures highlight how interruptions disrupt nurses' ability to perform essential tasks accurately. For example, in simulated IV push scenarios, nurses made significantly more errors when interrupted compared to when they worked without disruptions. Tara McCurdie from Healthcare Human Factors emphasizes the scale of this issue:
"nurses were interrupted every time they administered an IV push, sometimes more than once"
This reality underscores the constant challenge nurses face in clinical environments and reinforces the urgent need for systemic changes. Reducing interruptions is critical to safeguarding nursing workflows and enhancing patient safety.
Conclusion
The study highlights a clear link between IV line interruptions, patient safety risks, and nursing inefficiencies. Frequent interruptions not only disrupt workflows but also significantly increase the likelihood of clinical errors, ultimately affecting the quality of care and patient outcomes.
Interestingly, about 57.4% of these interruptions could be avoided. This opens the door for meaningful changes to shield nurses during critical activities like medication administration and IV line management. Strategies such as creating no-interruption zones, streamlining workflows, and addressing operational issues can help reduce errors and reclaim valuable nursing time.
Specialized tools also play a crucial role in reducing IV-related complications. For instance, the BeataClasp IV line organizer helps prevent line entanglement, accidental dislodgement, and keeps IV setups orderly. Considering that 68% of clinicians report accidental IV dislodgements occurring daily or multiple times a day, integrating securement devices like this into routine practice can significantly lower such risks. These tools enhance workflow stability while prioritizing patient safety.
Simulation studies further demonstrate the power of targeted interventions, showing a reduction in IV push errors from 89% to 32% and pump programming errors from 39% to 5%. These findings emphasize how a combination of protected work environments and the right tools can lead to safer care and more efficient nursing practices.
Ultimately, tackling IV interruptions is vital for ensuring safe and effective care. By combining environmental adjustments, standardized protocols, and innovative tools like the BeataClasp, healthcare facilities can create a safer and more reliable environment for both nurses and patients.
FAQs
How do interruptions to IV lines affect patient safety and nursing efficiency?
Interruptions to intravenous (IV) lines pose serious risks to patient safety and disrupt the flow of nursing tasks. Research shows that nearly half of all reported IV line errors result in harm that necessitates medical intervention. Common issues include incorrect infusion rates and IV lines being left unattached to patients. These errors are particularly concerning when high-alert medications are involved, as the consequences can be severe.
Frequent interruptions also place a heavy burden on nurses, increasing their cognitive load and making procedural mistakes more likely. Studies reveal that each interruption during medication administration raises the risk of errors and eats into valuable time. On average, nurses face eight interruptions during a standard 8-hour shift. Tools like BeataClasp's IV line organizer, designed to prevent line tangles, accidental disconnections, and contamination, can help address these challenges. By minimizing these risks, such tools enhance both workflow efficiency and patient safety.
What are the main causes of interruptions during IV line management?
Interruptions during IV line management often come from three main sources:
- Device alarms: Equipment like smart infusion pumps frequently trigger alerts that demand immediate attention, diverting nurses from their IV-related tasks.
- Environmental distractions: Everyday interruptions such as phone calls, text messages, or questions from colleagues and patients are common. In clinical settings, some studies have found nurses face as many as 13 interruptions per hour.
- Workflow demands: Routine responsibilities like documentation, preparing medications, or adjusting IV tubing often lead to task-switching, disrupting the flow of IV monitoring.
These disruptions can lead to increased mental fatigue, higher risks of line complications, and reduced efficiency. To address these challenges, strategies like minimizing unnecessary interruptions, managing alarm fatigue, and utilizing tools like the BeataClasp IV line organizer can help streamline processes and enhance patient safety.
How can healthcare teams reduce IV line interruptions to improve safety and efficiency?
Reducing interruptions with IV lines begins by establishing no-interruption zones around critical areas like the bedside or infusion pump. Simple steps such as posting clear signage and restricting access during IV setup can streamline the process and lower the chance of mistakes.
Adjusting workflows is another important step. Handling one infusion at a time, prioritizing medications that require extra caution, and clearly labeling lines can help cut down on disruptions. Staff training on proper pump setup and using tools like back-check valves can also make a big difference in keeping things running smoothly.
Keeping IV lines organized is equally important to avoid tangles, contamination, or accidental dislodgment. Tools like the Beata Clasp - a latex-free, antimicrobial IV line organizer - are designed to keep lines neat and secure, promoting both safety and efficiency during infusions.
