IV line safety is a critical concern in hospitals. Poor management can lead to patient injuries, infections, medication errors, and compliance issues. Key risks include tangled lines, contamination, and misconnections, which not only jeopardize patient outcomes but also increase costs and regulatory scrutiny.
To address these challenges, hospitals should implement evidence-based protocols, such as:
- Regular site rotation (every 72–96 hours) and daily monitoring for complications.
- Proper line organization to prevent tangling and misconnections.
- Accurate documentation of IV line placement, maintenance, and medication administration.
Tools like the Beata Clasp help streamline IV line management by keeping tubing elevated, organized, and sterile. Priced at $19.95 per unit, it reduces risks and saves time for healthcare providers.
Key Takeaway: Combining reliable protocols, clear documentation, and practical tools can improve IV safety, reduce complications, and enhance patient care.
How to Prime IV Tubing Line | How to Spike a IV Bag for Nursing
Evidence-Based Protocols for IV Line Management
Having reliable protocols in place is critical for reducing risks and ensuring patient safety in hospitals. Proper IV line management depends on adhering to proven methods that minimize complications and improve outcomes. These evidence-based practices offer healthcare teams clear instructions for maintaining safe and efficient IV therapy.
Standard Protocols for IV Therapy
Site selection and rotation: Following CDC guidelines, IV sites should be chosen and rotated every 72–96 hours. Upper extremity veins are generally preferred, with decisions based on vein quality, patient mobility, and the expected duration of treatment.
Pre-infusion risk assessments: Before starting therapy, assess for potential complications. This includes checking for allergies, ensuring medication compatibility, and evaluating vascular access needs. Always verify the "five rights" (right patient, drug, dose, route, and time) and review for possible drug interactions or contraindications.
Daily monitoring protocols: Shift assessments are essential to check for signs of infiltration, phlebitis, or infection. Look for redness, swelling, or patient-reported pain. Document these observations carefully to create a clear record of the IV line's condition and to track any emerging issues.
Protective dressings: Transparent dressings allow for easy inspection of the insertion site without the need for removal, reducing contamination risks. These dressings should be changed every 5–7 days or sooner if they become compromised. Always clean the site with chlorhexidine and ensure it dries completely before applying a new dressing.
Line organization: Secure IV tubing to prevent tension on insertion sites and avoid entanglement. Clearly label tubing with medication names, concentrations, and infusion rates. When managing multiple lines, organize them systematically to prevent confusion during medication administration or emergencies.
These protocols emphasize the importance of meticulous documentation, ensuring that all actions are recorded accurately and consistently.
U.S. Documentation Standards
Accurate and standardized documentation is essential for regulatory compliance and safe patient care. Proper records not only meet legal requirements but also help prevent dangerous errors.
Required documentation elements: Record the insertion date and time, site location, catheter gauge and length, number of insertion attempts, and the name of the healthcare provider performing the procedure. Use MM/DD/YYYY for dates and a 12-hour format with AM/PM for times. Any complications or patient reactions must be documented immediately, including symptoms, interventions, and patient responses.
Medication administration records: Document infusion rates, total volumes administered, and any changes in rates during therapy. Use standard U.S. measurements like milliliters (mL) and liters (L) for fluid volumes, and record infusion rates in mL/hour. If there are deviations from prescribed rates, provide a clear explanation in the medical record.
Shift-to-shift communication: Thorough documentation of IV line assessments, site conditions, and any concerns is vital for seamless handoffs between shifts. This aligns with The Joint Commission's standards for effective communication and helps prevent information gaps that could compromise patient safety. Electronic records should be used to provide real-time updates on IV line status.
Temperature monitoring for medications requiring controlled storage should be recorded in Fahrenheit, as per U.S. healthcare standards. Any temperature deviations must be reported and documented according to facility policies and FDA guidelines to ensure medication safety.
Nurse-Led Best Practices for Safe IV Line Organization
Nurses play a vital role in maintaining patient safety, particularly when it comes to managing IV lines. Their practical, hands-on experience informs strategies that help minimize complications and streamline clinical workflows.
Methods for Reducing Line Entanglement
To prevent IV line mix-ups, use clear, waterproof labels and incorporate color coding when necessary for quick identification. Proper labeling reduces confusion and ensures smoother care.
Securing IV tubing with medical tape at key points and alternating the placement of multiple lines can help minimize tension on catheters and prevent tangling. This simple step not only keeps lines organized but also reduces the risk of accidental dislodgement.
Keeping IV tubing elevated and off the floor is another critical practice. Devices like bed-mounted hooks or clips can keep excess tubing raised, maintaining sterility and preventing contamination - whether the patient is lying down or walking around.
Regularly inspecting IV lines for issues like kinks or improper positioning allows for timely adjustments, ensuring that tubing remains functional and sterile.
Hygiene and Aseptic Techniques
Effective IV line management goes hand in hand with strict hygiene practices. Always perform hand hygiene before and after any contact with IV systems. When accessing ports, wear sterile gloves, disinfect injection sites with antiseptic, and ensure sterile supplies remain sealed until use.
Maintaining aseptic techniques is non-negotiable. This includes using sterile gloves when accessing IV ports or changing dressings and disinfecting injection ports with antiseptic, allowing them to dry completely before proceeding. These steps are essential for infection control in clinical settings.
The environment also plays a role in maintaining sterility. Procedures should be performed in low-traffic, well-lit areas to reduce the risk of contamination.
Room Safety and Workflow Adjustments
Creating a safe and organized patient environment is another layer of protection. Proper patient positioning can ease strain on IV sites while improving comfort. Adjusting posture so that IV lines follow natural body contours and supporting the limb with the IV can improve circulation and reduce discomfort.
Place IV poles and supplies within easy reach but ensure they are secure to prevent accidental dislodgement. Arrange furniture to create clear pathways, keeping IV lines free from interference. Regular safety checks of the patient’s immediate surroundings can help identify loose connections or hazards early.
Clear communication among the care team is equally crucial. Tools like bedside whiteboards or detailed handoffs during shift changes ensure every nurse is up to date on IV management plans and patient-specific considerations. This collaborative approach enhances consistency and promotes overall safety.
sbb-itb-f779e18
Tools for IV Line Safety: Spotlight on Beata Clasp
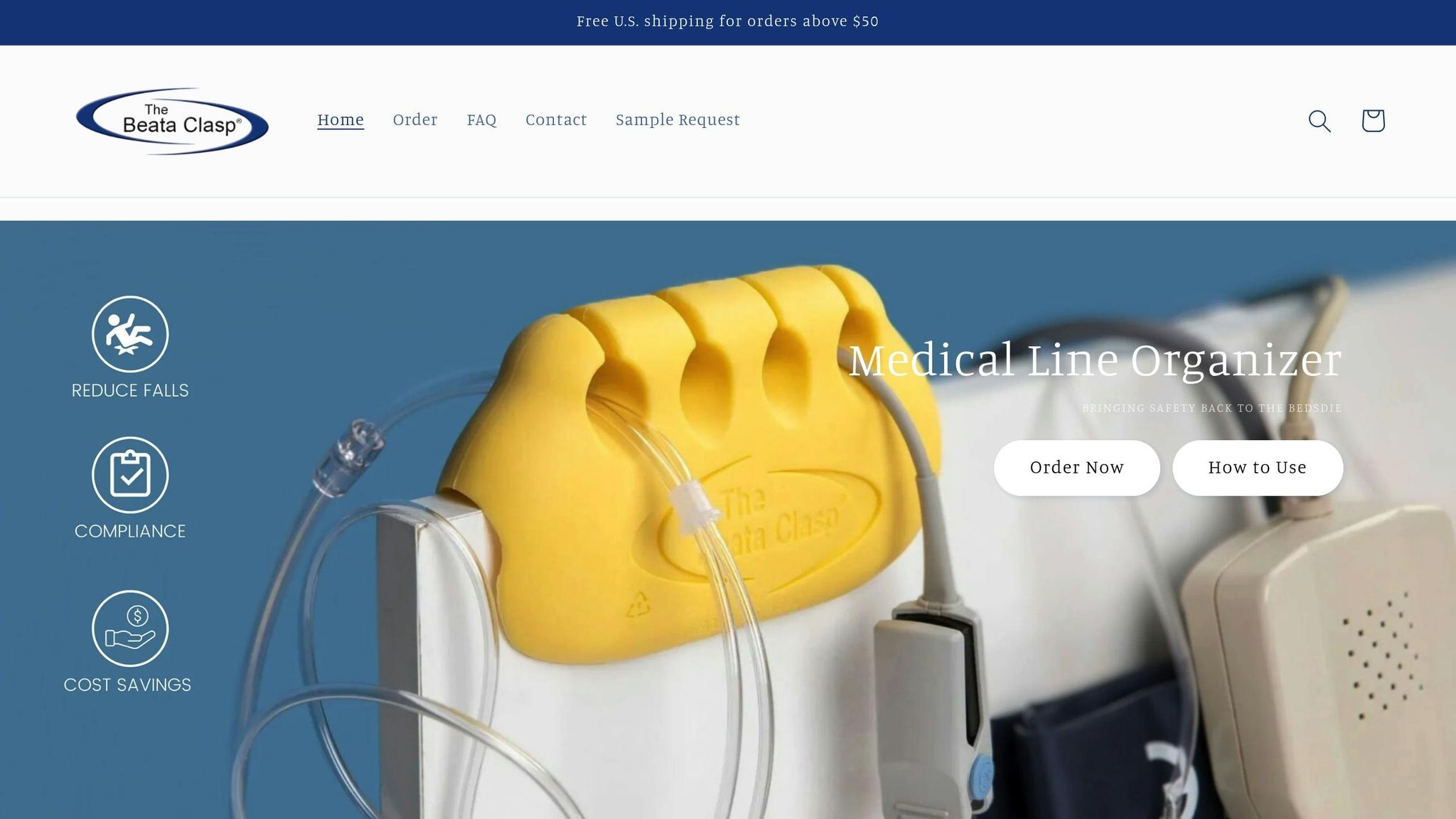
When it comes to IV line management, having the right tools alongside solid protocols can make a world of difference. The Beata Clasp is one such tool, created by nurses who understand the everyday challenges of IV line management in healthcare settings. This practical device seamlessly integrates into existing workflows, helping to prevent complications and simplify the process.
Core Features and Benefits
The Beata Clasp is designed with safety and efficiency in mind. Its antimicrobial, latex-free, and adhesive-free construction helps control infections while avoiding the residue or skin irritation often associated with tape-based solutions.
One standout feature is its ability to keep tubing elevated and organized, reducing the risk of tangling without adding extra steps for caregivers. This streamlined design minimizes hazards like trips and falls, protecting both patients and healthcare workers. By addressing these common issues, the Beata Clasp enhances daily IV management in measurable ways.
The device's high-alert color ensures that IV lines are easily identifiable during emergencies or routine care. From a workflow perspective, it saves time by eliminating the need to untangle or reposition tubing, allowing nurses to focus more on patient care and less on managing equipment.
Additionally, the Beata Clasp is easy to clean and features an antimicrobial surface, supporting strict infection control measures. Its recyclable materials align with sustainability goals, and it can be used for single or multiple patients, making it a versatile option for various healthcare settings.
Use Cases in Healthcare Settings
The Beata Clasp proves its value across a range of healthcare environments:
- Intensive Care Units (ICUs): In ICUs, where patients often have multiple IV lines, the device helps prevent misconnections by keeping lines neatly organized. This is especially beneficial when managing complex medication regimens that require frequent access to IV lines.
- Medical-Surgical Units: For patients recovering in medical-surgical units, the Beata Clasp enhances mobility. By keeping IV lines organized, it reduces the risk of accidental dislodgment, making walking safer for both patients and staff.
- Home Healthcare: In home care settings, where family members or patients manage IV therapy, the Beata Clasp’s straightforward design requires no special training. It delivers professional-level safety benefits in a simple, user-friendly way.
- Emergency Departments: During high-pressure situations in emergency departments, the device’s quick identification feature allows multiple providers to locate and access the correct IV lines swiftly, ensuring timely interventions.
Pricing and Availability
The Beata Clasp is offered with flexible pricing options to suit different needs:
- Individual Units: Priced at $19.95 each, ideal for smaller practices or home healthcare use.
- Evaluation Pack: A set of 10 units is available for $163.00, allowing facilities to test the product before committing to larger orders.
- Bulk Orders: For broader implementation, facilities can purchase 25 units for $467.50. This cost-effective option supports efficient workflows and improved patient safety, especially given the device’s reusability.
With its thoughtful design and practical pricing, the Beata Clasp is a smart addition to any healthcare setting aiming to improve IV line safety and efficiency.
Workflow Improvement and Risk Reduction Methods
Ensuring IV line safety requires more than just following guidelines - it’s about seamlessly integrating effective tools and practices into everyday routines. By combining established protocols with nurse-led strategies, hospitals can turn safety measures into habits. Technology, training, and continuous monitoring play a critical role in embedding these practices into daily workflows.
Using Digital Tools and Checklists
Digital tools like EHR prompts, mobile checklists, and barcode scanning systems help healthcare teams stay on top of IV line safety. These tools reduce mental strain while ensuring consistent adherence to safety protocols. For example, mobile checklists allow nurses to scan QR codes on IV equipment, giving them instant access to patient-specific protocols. This minimizes confusion around medication compatibility, infusion rates, and maintenance schedules. When paired with tools like the Beata Clasp, these systems create an organized and efficient approach to managing IV lines.
Barcode scanning technology adds another layer of safety by verifying correct IV line connections before administering medications. However, for this to work effectively, IV lines must be well-organized. Tangled or disorganized tubing can complicate the scanning process and increase the chance of errors.
Real-time dashboards provide a bird’s-eye view of IV-related incidents across hospital units. Charge nurses can use these dashboards to spot trends, such as higher rates of line dislodgment or infections, and make informed decisions about staffing or protocol adjustments. These metrics also shed light on how much time is spent on IV line management, offering valuable insights for workflow optimization.
Regular Audits and Staff Training
Monthly safety audits conducted by infection control teams are essential for maintaining high standards in IV line management. These audits don’t just check for hand hygiene compliance - they also assess how well IV lines are secured and organized to reduce contamination risks. Facilities that prioritize regular audits often see a noticeable drop in IV-related complications.
Ongoing training ensures that staff remain proficient in the latest IV line management techniques. Competency-based programs include hands-on demonstrations, where nurses practice proper line organization and learn how to use safety tools effectively. Real-life scenarios are often incorporated, allowing nurses to manage multiple IV lines while balancing patient care and mobility.
Peer mentorship programs are another effective way to reinforce safe practices. Pairing experienced nurses with newer staff creates opportunities to address workflow challenges that might not surface during formal training. Mentors can also demonstrate how tools like the Beata Clasp fit into daily routines, making it easier for new staff to adopt these practices.
Simulation exercises that replicate emergency situations provide valuable practice for managing IV lines under pressure. These drills not only improve emergency response times but also enhance overall efficiency in patient care.
Preventing Adverse Events with Early Action
Preventing IV-related complications starts with identifying patients who are at higher risk. Factors like limited mobility, multiple IV therapies, or cognitive impairments can signal the need for closer monitoring and better line organization.
Early warning systems integrated into EHRs can flag potential issues based on documentation patterns. For instance, if records suggest recurring problems, the system can prompt additional reviews or safety measures to address the risks.
Clear communication during shift handoffs is another critical step in preventing adverse events. Standardized protocols ensure that information about IV line organization and patient-specific needs is passed along accurately. This includes details about tools being used and any unique considerations for managing the patient’s lines.
Root cause analyses of IV-related incidents focus on understanding not just what went wrong but also how better tools and workflows could prevent similar issues in the future. These reviews often highlight that even small problems - like tangled tubing or unclear labeling - can escalate into significant safety concerns. By addressing these details proactively, hospitals can strengthen patient safety and reduce risks across the board.
Conclusion: Creating Safer Hospital Environments Line by Line
Improving hospital safety happens step by step, and effective IV line management is a key part of that journey. By following evidence-based protocols and embracing nurse-led practices, healthcare teams can create safer spaces for both patients and staff. Adding to these strategies, a well-organized physical setup plays a crucial role in enhancing safety.
When IV lines are neatly arranged and supported by practical tools, nurses can quickly address potential issues, improving efficiency and reducing stress. Clear identification of lines, prevention of tangles, and maintaining sterile conditions allow nurses to spend less time troubleshooting and more time focusing on patient care.
While digital tools and ongoing training are vital, the physical organization of IV lines should not be overlooked. Products like the Beata Clasp tackle the challenge of keeping lines orderly and accessible. At just $19.95 per unit, it offers an affordable way to support patient safety and avoid costly complications.
Small, consistent improvements in daily routines can have a big impact on overall safety. A single tangled line might seem like a minor issue, but when multiplied across hundreds of patients and thousands of interactions, the consequences can be significant. Addressing these small details systematically helps create an environment where safety becomes second nature rather than an added responsibility.
FAQs
How do evidence-based protocols help improve IV line safety in hospitals?
Evidence-based protocols are essential for boosting IV line safety, as they set clear and standardized practices. These guidelines help minimize risks like medication errors, infections, and other complications, which directly contributes to better patient outcomes.
By offering consistent instructions for inserting, maintaining, and removing IV lines at the right time, healthcare teams can perform procedures more safely and streamline their workflows. These nurse-led approaches not only improve hospital safety but also elevate the quality of care patients receive.
How does the Beata Clasp improve IV line management and patient safety in hospitals?
The Beata Clasp offers a straightforward solution for managing IV lines by keeping them neatly organized and tangle-free. This not only helps maintain a cleaner, safer environment for patients by reducing the risk of infections but also ensures that lines stay off the floor, enhancing overall hygiene.
By eliminating the hassle of tangled or misplaced lines, the Beata Clasp allows healthcare professionals to work more efficiently. Its user-friendly design saves time, minimizes disruptions, and lets medical staff concentrate on what matters most - providing quality patient care.
Why is accurate documentation important for managing IV lines and ensuring patient safety?
Accurate documentation plays a key role in managing IV lines. It creates a detailed record of when and how vascular access devices are inserted, assessed, and maintained. This clarity helps reduce risks like infections or improper line management, directly contributing to patient safety and seamless care.
It’s not just about patient care, though. Proper and timely documentation also safeguards healthcare professionals and hospitals. It serves as a reliable reference during audits or if adverse events occur. Beyond compliance, it supports clinical decisions and streamlines workflows, paving the way for improved results in hospital settings.
