IV tubing errors can be dangerous, but there’s a solution. Managing tangled lines, misconnections, and unclear labeling often disrupts care and puts patients at risk. The Line Management and Alignment Protocol (LMAP) addresses these issues with practical steps nurses can use immediately, improving safety and efficiency without expensive tools.
Key Highlights:
- Dual-location labeling ensures lines are clearly marked at both the pump and insertion site.
- Color-coded labels (e.g., red for arterial, blue for venous) make identification faster.
- Systematic tracing reduces misconnections and errors.
- Bedside organization minimizes tangles and delays.
Paired with tools like the Beata Clasp, which keeps IV lines organized and visible, LMAP simplifies workflows and enhances patient care. Starting at $19.95, these solutions are affordable and effective for facilities of any size.
In the Know with RNAO Multiple IV Infusion Safety and Nursing Education Implications 20150629 1600 1
Key Components of the Line Management Protocol (LMAP)
The Line Management Protocol (LMAP) builds on well-established IV safety practices in U.S. healthcare by focusing on standardized line tracing and labeling. These methods are designed to prevent misconnections and improve patient safety. By providing a clear, structured approach, LMAP also helps lighten the workload for nurses, aligning with the "five rights" of medication administration: the right patient, drug, dose, route, and time. Below, we break down the specific labeling strategies that are central to LMAP.
Standard Line Tracing and Labeling Methods
At the heart of LMAP is dual-location labeling, which involves placing labels at both the insertion site and near the pump or infusion device. This method creates multiple points for verification, allowing nurses to visually confirm connections without the need for lengthy tubing tracing.
To further streamline the process, color-coded labels are used to distinguish between different line types. For example:
- Red labels mark arterial lines.
- Blue labels indicate venous access.
- Purple labels are for enteral feeding tubes.
- Yellow labels denote epidural lines.
This color-coding provides an immediate visual cue, reducing the risk of misconnections and simplifying line identification.
Each label includes essential information such as the drug name, concentration, route, and patient details. Designed for clarity and durability, these labels remain legible throughout the course of therapy, helping to minimize errors and ease cognitive strain during busy or high-pressure scenarios.
Lastly, LMAP underscores the importance of systematic verification. Nurses are guided to follow a consistent pathway from the pump to the patient, checking each connection point along the way. This step-by-step process ensures any potential misconnection is identified and corrected before it can impact patient care.
Step-by-Step Guide for Using LMAP in Clinical Practice
Integrating LMAP into everyday clinical workflows ensures a smoother process and enhances patient safety. This protocol builds on existing labeling and tracing practices, offering a structured approach for nurses to follow consistently.
Bedside LMAP Application
The bedside use of LMAP starts with an initial line assessment during shift handoff. Nurses should identify all active lines by reviewing existing labels and comparing them against the patient’s current medication orders. This step helps catch potential errors before they escalate.
Next, line verification involves tracing each line from the infusion pump to the patient’s access point. Nurses should carefully check all critical connection points, including the pump connection, any inline filters or extension sets, and the final access site.
For new lines, apply dual-location labels immediately to ensure accuracy. Placing labels in two spots ensures they remain visible, even if the patient is repositioned or if multiple lines create visual clutter.
All line placements and verifications should be documented in real-time within the electronic health record. This ensures accurate, up-to-date information is available for the next nurse performing their LMAP assessment.
The protocol also emphasizes bedside organization. Lines should be arranged neatly, avoiding unnecessary crossing, and similar line types should be grouped together when possible. This physical organization enhances visibility and makes the color-coding system more effective.
Communication Tools and Checklists
Beyond bedside procedures, clear communication is vital for maintaining safety and continuity.
LMAP depends on standardized handoff communication. During shift changes, the outgoing nurse should verbally confirm each line’s purpose, medication, and any recent changes while the incoming nurse visually traces the line. This dual verification process reduces the risk of errors that might slip through written reports.
Digital checklists within electronic health records prompt nurses to verify line placement, check label accuracy, and confirm proper alignment before documenting their work. These tools also allow for real-time tracking of compliance and help identify areas where additional training may be needed.
When issues arise, escalation protocols provide clear guidance. If a nurse encounters unlabeled lines, mismatched medications, or uncertainty about line placement, they must immediately consult the charge nurse or attending physician. This prevents assumptions that could jeopardize patient safety.
At the nursing station, team communication boards display LMAP compliance rates and highlight recent safety events related to line management. These visual tools keep safety at the forefront and encourage accountability for following the protocol.
For high-risk scenarios like patient transfers, post-procedure returns, or new emergency department admissions, standardized communication templates outline exactly what details must be shared and in what order. These templates help ensure no critical information is overlooked during fast-paced transitions.
While LMAP provides a solid framework for safer line management, pairing it with the right physical tools can take its effectiveness to the next level. Tools that complement LMAP's core practices can transform bedside line management, making care more seamless and efficient.
One such tool is the Beata Clasp, designed to align with LMAP's emphasis on clarity and organization. This soft, recyclable foam clasp attaches directly to hospital bedrails, offering a simple, adhesive-free way to keep IV lines organized. By eliminating the need for permanent fixtures, it provides a flexible and practical solution to common IV line management challenges.
Beata Clasp Features and Benefits
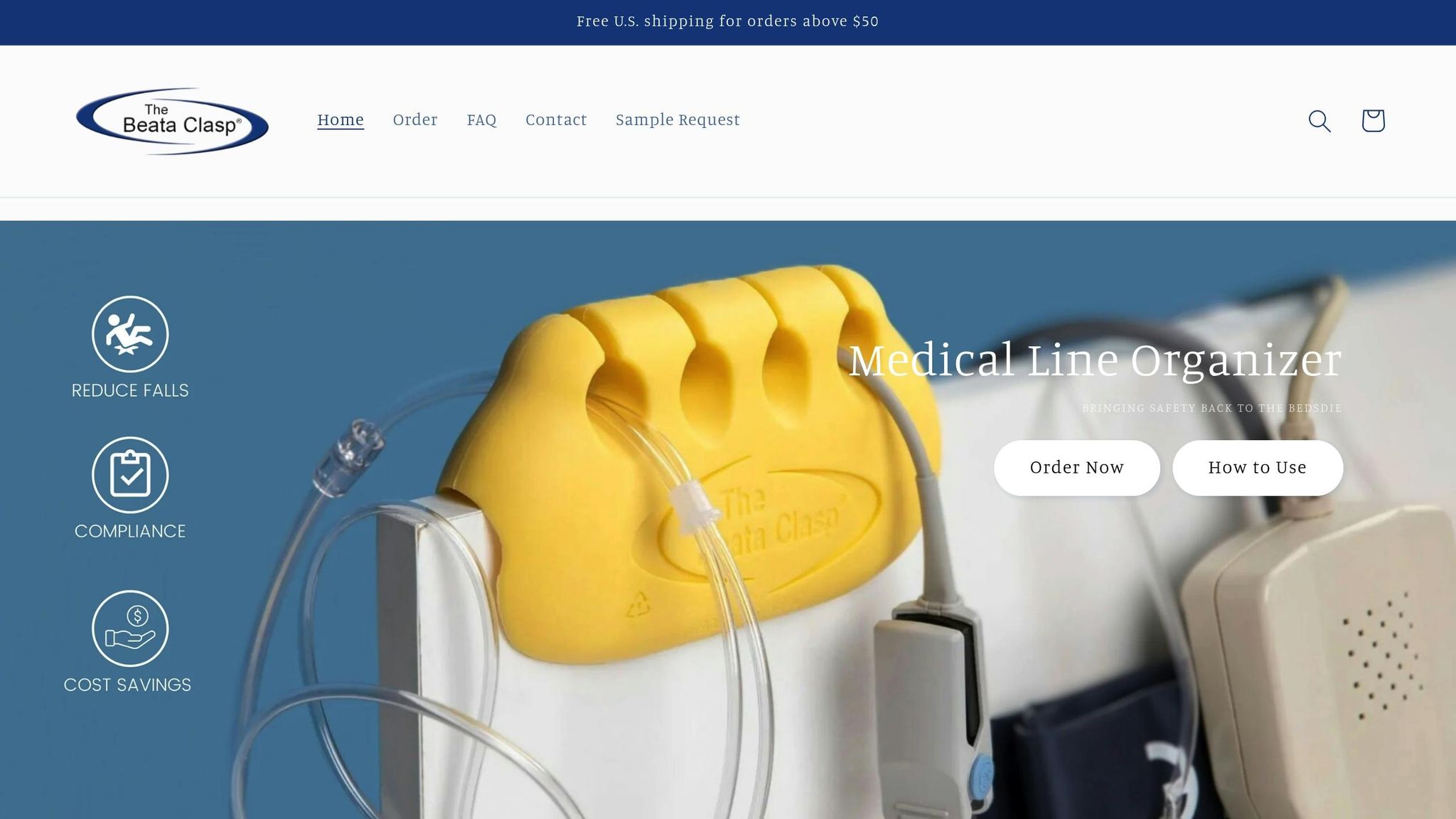
The Beata Clasp is a practical addition to support LMAP's goals of safety and efficiency. Here’s what it offers:
- Antimicrobial properties help minimize contamination during frequent adjustments.
- Adhesive-free design allows easy repositioning without leaving residue.
- High-alert coloring ensures lines are easy to spot in any lighting condition.
- Keeps IV lines organized, reducing tangles and supporting color-coding systems.
- Latex-free construction makes it safe for patients with latex sensitivities, ensuring broad compatibility.
- Easy-to-clean surface meets infection control standards and works with common hospital disinfectants.
By maintaining consistent organization, the Beata Clasp can streamline nurse handovers and improve transitions of care.
sbb-itb-f779e18
Pricing Options for U.S. Healthcare Settings
Healthcare facilities can choose from several pricing options tailored to their needs:
| Option | Price | Best For | Cost Per Unit |
|---|---|---|---|
| Individual Unit | $19.95 | Single patient rooms or pilot testing | $19.95 |
| Evaluation Pack | $163.00 | Small units assessing initial feasibility | $16.30 |
| Bulk Order | $467.50 | Large facilities implementing system-wide | $18.70 |
For pilot testing, the Individual Unit is ideal. Small units can opt for the Evaluation Pack, which includes 10 units at a reduced cost per unit. Facilities planning a full-scale rollout can benefit from the Bulk Order option.
Results of LMAP Adoption in U.S. Healthcare
Healthcare facilities across the United States have seen measurable gains in patient safety after adopting the Line Management and Alignment Protocol (LMAP). This approach has brought tangible improvements, particularly in key areas directly tied to patient safety.
Fewer Risks and Errors
With its standardized protocols, LMAP has significantly minimized incidents of line entanglement, which helps reduce patient falls and accidental disconnections. Additionally, consistent tracing and clear labeling practices have cut down on misconnection errors, boosting the safety of IV line management overall.
Conclusion: Simplifying Tubing Safety with LMAP
LMAP takes tubing safety to the next level by standardizing tracing and labeling processes, which helps minimize administration errors and makes IV line identification much more straightforward. Paired with tools like the Beata Clasp - designed with antimicrobial features and a high-alert color scheme - LMAP supports better decision-making in high-pressure situations.
With pricing starting at $19.95 and bulk purchase options available, healthcare facilities across the U.S. can quickly adopt these solutions to address tubing-related risks. By integrating LMAP and the Beata Clasp, hospitals can achieve safer and more efficient patient care, ensuring a more reliable clinical environment.
FAQs
How does the Line Management and Alignment Protocol (LMAP) enhance patient safety in clinical settings?
The Line Management and Alignment Protocol (LMAP) improves patient safety by establishing clear and standardized procedures for handling IV lines. This includes proper routing of lines, ensuring secure connections, and providing comprehensive staff training. Together, these steps help reduce risks such as misconnections, dislodged lines, and tangled tubing.
By addressing these issues, LMAP helps prevent medication errors, lowers the chances of infections, and streamlines workflows. This not only creates a safer environment for patients but also makes it easier for healthcare professionals to provide top-notch care.
How do color-coded labels improve IV line management and enhance patient safety?
Color-coded labels are a game-changer when it comes to managing IV lines. They provide an easy visual system to identify different lines, significantly reducing the chances of mistakes like connecting the wrong line or giving the wrong fluids or medications - errors that could seriously jeopardize patient safety.
In fast-paced or complicated clinical settings, these labels make it much simpler to quickly verify and differentiate lines. This not only boosts workflow efficiency but also frees up healthcare professionals to concentrate on delivering precise, safe care. The result? Less time spent on troubleshooting and a greater focus on improving patient outcomes.
How can healthcare facilities use Beata Clasp with LMAP to improve tubing safety and organization?
Healthcare facilities can improve tubing safety and organization by using the Beata Clasp alongside the Line Management and Alignment Protocol (LMAP). The Beata Clasp helps keep tubing neatly arranged, reducing the chances of tangles or incorrect connections. This combination creates a safer and more efficient process for managing lines in clinical environments.
Integrating the Beata Clasp into LMAP practices allows healthcare teams to standardize how tubing is handled. This makes it easier for nurses to manage even the most complex setups, cutting down on mistakes, enhancing patient safety, and simplifying daily workflows.
